Management

Tsukayama Classification

Subscapularis failure
Rotator cuff failure
Instability
Infection
Periprosthetic fracture
Aseptic loosening
Neurological injury
Parada et al. J Should Elbow Surg 2021
- 2224 aTSA complication rate 11%, revision rate 5.6%
- haemarthrosis
- DVT
- infection



Incidence
Peters et al J Arthroplasty 2009
Knee > Hip
- superficial position
- limited cover of well vascularised muscle
- watershed area of skin blood supply anterior to the skin incision
- much increased in fully constrained prosthesis
Ideal < 1%
Increased with
- revision
- prior infection
- RA / Psoriatic arthropathy
- DM
Identify high risk groups
- immunocompromised
- diabetes
- RA
- malnutrition
Urine screen
- check for and treat UTi
Groin, nose, axilla swabs
- for MRSA
- if positive, treat
- need 3 consecutive free swabs
3 x chlorhexidine preoperative showers in 8 hours
Admit day of surgery
- check skin for lesions
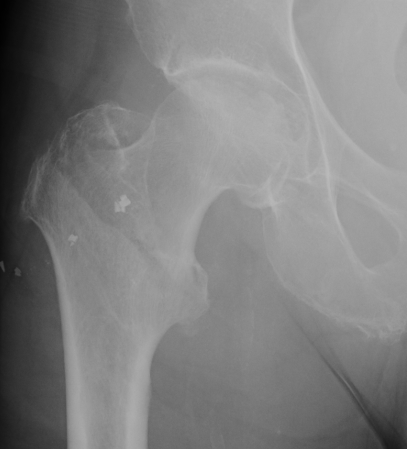
Fracture which extends between the trochanters of the proximal femur
- lower limit is inferior border of lesser tuberosity
Extra capsular / well vascularized
The key to stability is the posteromedial cortex