
Goals of femoral cementing
Optimize cement-bone interface
Cement mantle free of defects
Minimum 2 mm thickness
Femoral component centered in cement mantle
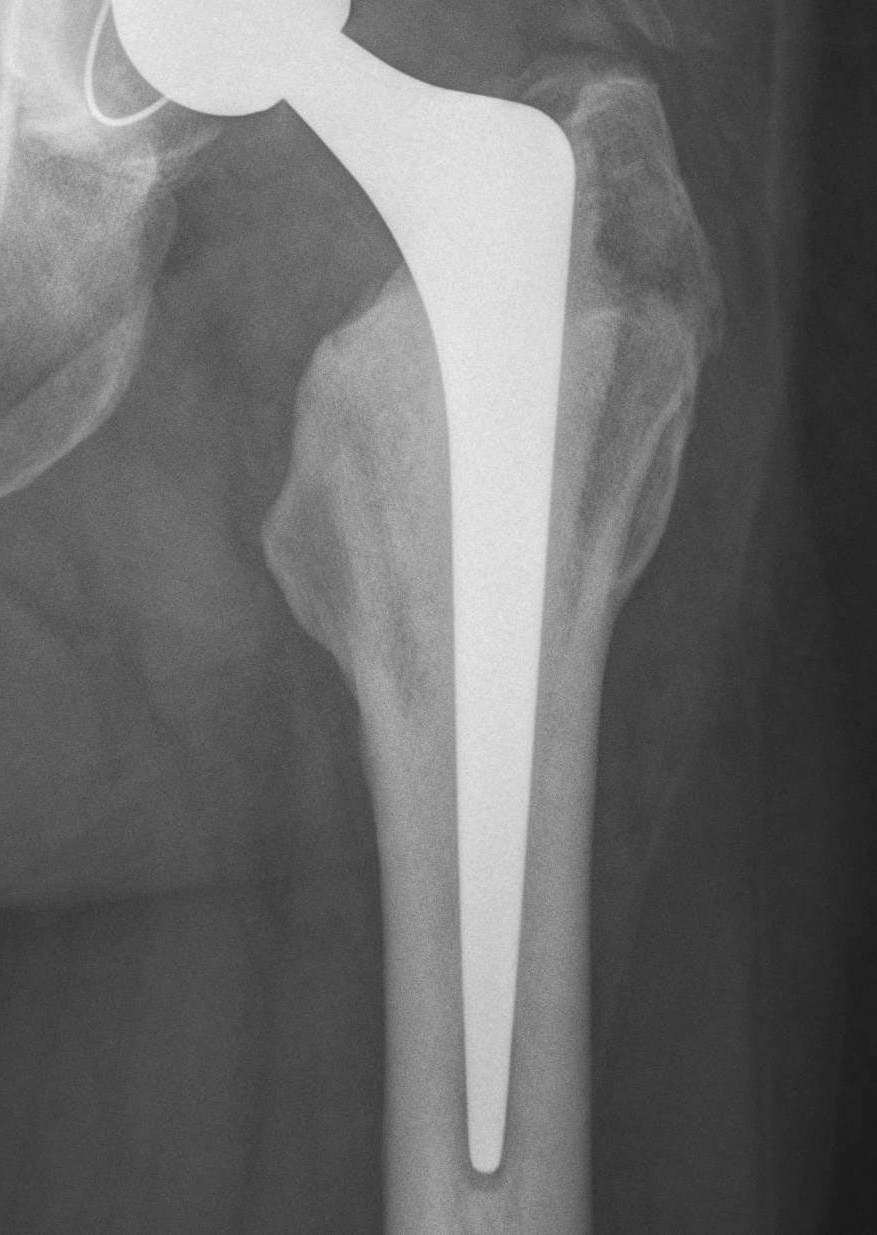
Design


Styker Exeter Stem Zimmer CPT
Polished surface
- Ra less than 1 micrometer
- polished stems create little abrasion
- allow subsidence and keep cement in compressive loading
Taper
- double or triple taper
- behaves as a Morse taper in the cement mantle
- allows controlled subsidence within the cement
Collar
- may reduce stress shielding of proximal femur & reduce strain in proximal medial cement mantle
- prevents subsidence
Material
- Cobalt-chromium alloy stems
- generate less particulate debris than titanium
Cement Issues

Cement viscosity
- structural superiority of high viscosity over low viscosity cement
- i.e. Simplex (highly viscous) v Palacos (low viscosity)
Centriguation / vacuum mixing
- reduces pore size
- stronger cement
- more resistant to fracturing
Pressurization
- pressurization increases penetration
- increases strength of cement-bone interface
Centralisers
- achieve more uniform cement mantle
- especially in zone 5 & 6
Cement Mantle
- crack incidence greatest when mantle < 2 mm
- varus stem results in thin cement mantle in proximal medial & distal lateral zones
Antibiotics
- in relatively small doses effect on mechanical characteristics of PMMA negligible
- must be heat labile
- vancomycin / tobramycin / gentamicin
Cementing techniques
First-generation
- finger-packing doughy cement
Second-generation
- cement restrictor
- cleaning with pulsatile lavage
- cement inserted retrograde using cement gun
Third-generation
- vacuum centrifuge (reduce porosity)
- pressurization of cement mantle
Barrack's femoral component cementation quality grading system
| Grade | Definition |
|---|---|
| A | Complete filling of the medullary canal, without radiolucent lines between the cement and the bone (white-out) |
| B | Radiolucent line covering up to 50% of the cement-bone interface |
| C | Radiolucent line covering between 50% and 99% of the cement-bone interface or incomplete cement mantle |
| D | Complete radiolucent line (100%) at the cement-bone interface and/or absence of cement distally to the end of the stem |

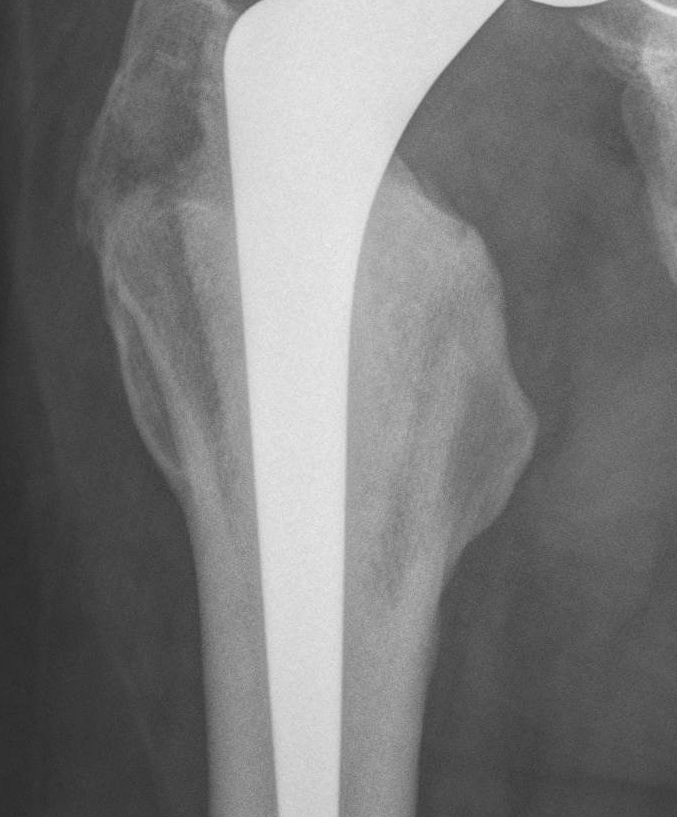

Grade A Grade B Grade C Grade D
Techniques
Stryker Exeter surgical technique PDF
Zimmer CPT surgical technique PDF
Results
Australian Joint Registry 2023 Revision rates by fixation (400,000 THA)
| Cemented | Uncemented | Hybrid | |
|---|---|---|---|
| 5 year | 2.6 | 3.0 | 2.6 |
| 10 year | 3.8 | 4.3 | 3.9 |
| 15 year | 5.1 | 5.9 | 5.3 |
| 20 year | 7.0 | 6.7 |
15 year revision rate by age
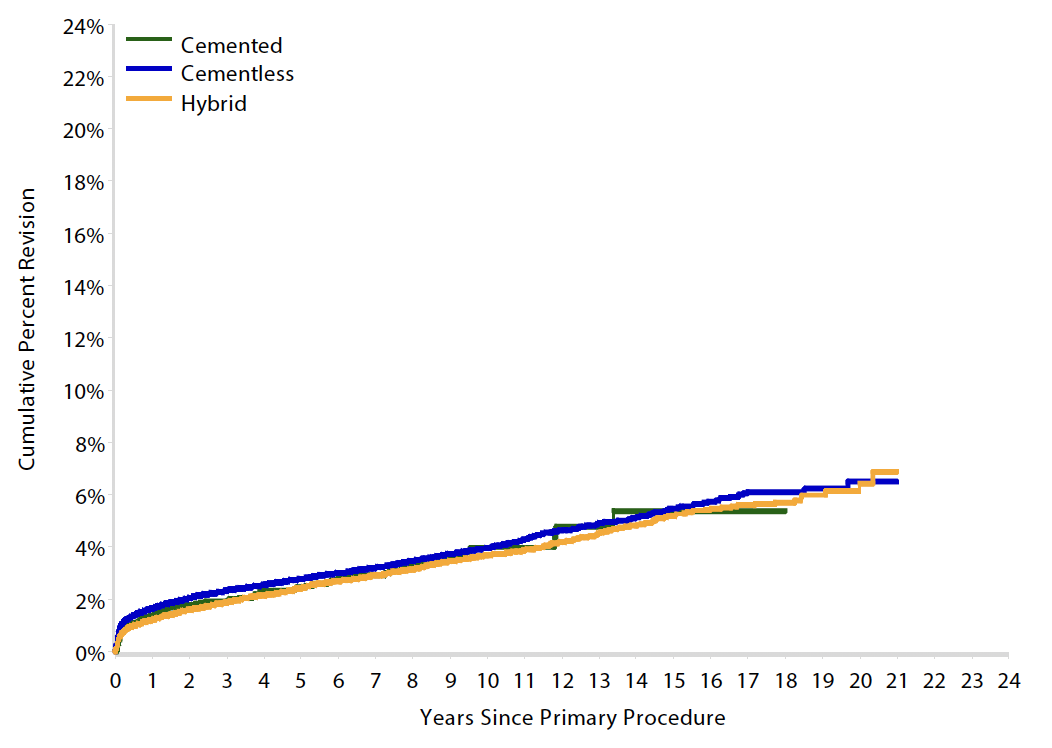
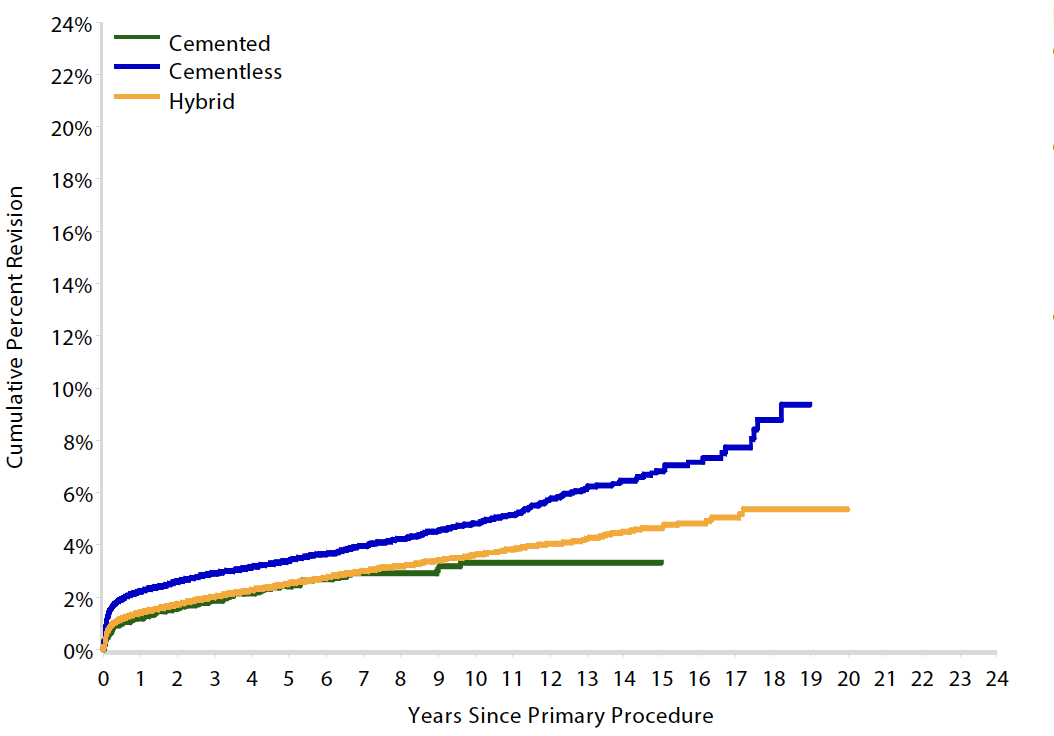
64 - 74 year > 75 years
| Cemented | Uncemented | Hybrid | |
|---|---|---|---|
| < 55 | 6.4 | 7.2 | |
| 55 - 64 | 6.2 | 5.5 | 6.1 |
| 65 - 74 | 5.4 | 5.5 | 5.2 |
| > 75 | 3.3 | 6.8 | 4.7 |
Complications
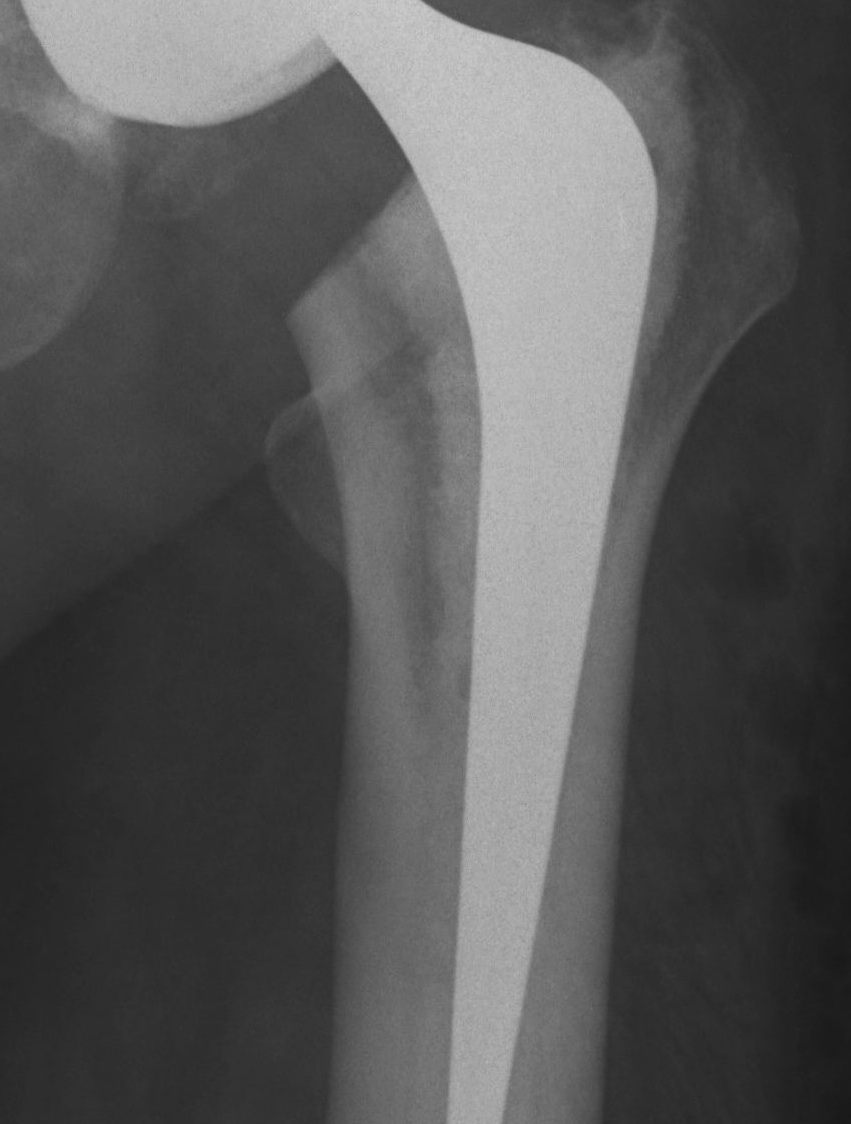
Loosening
Harris Categories of Cemented Femoral Stem Loosening
| Definitely Loose | Probably Loose | Possibly Loose |
|---|---|---|
|
Change in stem position
Cement mantle fracture
Radiolucent line > 1 mm |
Lucencies at cement implant interface
Endosteal scalloping |
Radiolucent lines at cement/bone interface |


Definitely Probably Possibly
