Pathological Processes
Two possible types of injury
1. Axonal
2. Myelin sheath
Myelin Sheath Damage
Causes
Commonly seen in compression
- i.e. CTD, ulna nerve at elbow
- area of focal demyelination
Can progress to a conduction block
- some or all axons simply stop working
- decreases the amplitudes
Effect
1. Usually affects sensory fibres first
- affects motor fibres later
2. Results in slowing of conduction velocity
3. Prolonged distal latency
- i.e. long time for stimulation to reach recording electrodes
4. Effect is focal
- slowed conduction velocity above block
- normal below
- can isolate level of entrapment
5. If progresses to conduction block
- decreased amplitude
Axonal Damage
Cause
Due to severe damage to the axon
- laceration / avulsion / severe contusion i.e. Sunderland type 3 and 4
Effect
1. Decreased amplitude - related to number of axons affected
2. Normal latency and conduction velocity
3. In contrast to demyelination, cannot get normal result by stimulating below level of lesion
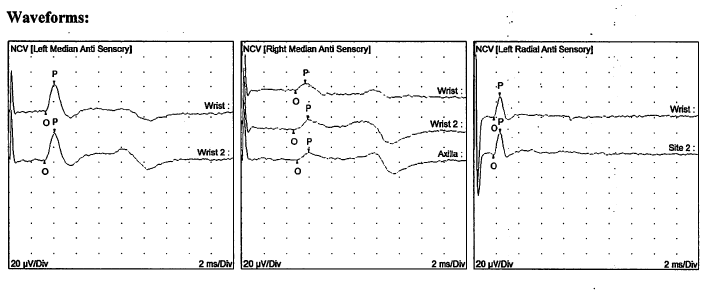
SNAP
Definition
Sensory nerve action potentials
Technique
Stimulate a sensory nerve and measure the action potential distally
Median nerve
- two stimulations over median nerve in forearm (S)
- ring type recording (R) electrodes on index and middle finger (sensory nerves only)
Ulna nerve
- stimulation over ulna nerve at elbow or wrist
- record over little finger
Measure
Latency
- time to reach distal electrodes
Conduction velocity
- simply measure distance between electrodes
- computer calculates velocity
Amplitude
- number of axons being stimulated
- also need all the axons transmitting at a similar velocity or get a wide, shorter velocity
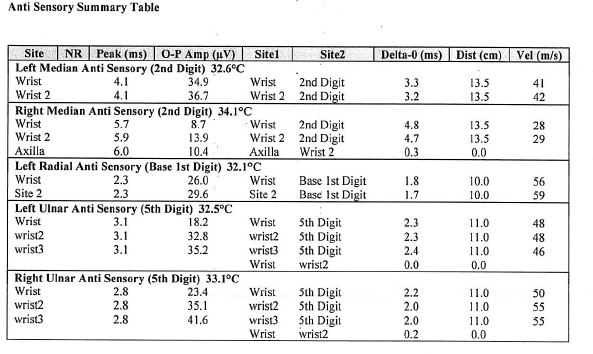
Uses
Diagnosis of carpal tunnel syndrome
- measure conduction velocity
- in upper limb is usually > 50 m/s
- compare to ulna nerve / standard charts
- median nerve is slower than ulna, but difference should be < 0.2 ms
- usually use 0.3 ms as cut off
Ulna nerve compression
CPN compression
Radial nerve
Sciatic nerve
CMAP
Definition
Combined motor action potential
- called this because is difficult to stimulate just one muscle
- i.e. on thenar eminence want to stimulate just APB, but would get FPB also
Technique
Stimulate a nerve and record from a muscle that it innervates
Measure
1. Distal latency
2. Conduction velocity
- stimulate at 2 points and measure difference between times
- 50 m/s UL
- 40 m/s LL
3. Amplitude
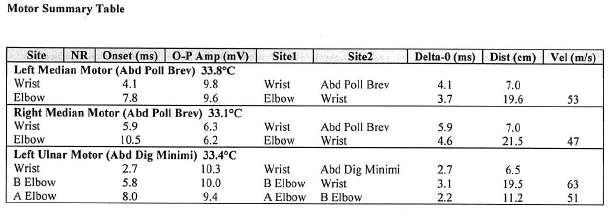
Uses
Same as for SNAP
- entrapments
- slowing of conduction velocity and latency with demyelination
- +/- decreased amplitude if any axonal damage (severe entrapment, traumatic contusions, lacerations)
MNAP
Principle
Combine sensory and motor
- measuring electrodes simply in palm in median nerve distribution
- measure sensory and motor components
- see in delayed latency or conduction velocity
- very simple for CTD
- can move onto more specific SNAP and CMAP if needed
Responses
Amplitude
Proportional to number of functional axons
- loss of axons causes decrease in response amplitude
- amplitude is a measure of the total number of functioning axons in the nerve
Conduction Velocity
Calculated fro
m the latency values
- reflects only the function of the fastest conducting fibres
- fortunately most compressive or traumatic disorders affect the largest fibres
Calculated by
- dividing the latency by the distance between the stimulating and recording electrodes
Problem in CMAP
- the response is measured over the muscle
- the delay at the motor end plate must be considered
- conduction slowed by the small, unmyelinated terminal branches of the motor axon
- and by the time taken for release of Ach
- typically ~1 mS
- because the delay is fairly constant the terminal latency can be compared with the range of normal values
The Late Responses
Uses
Nerve root or proximal nerve lesions
- cannot use simple NCS
- stimulate a peripheral nerve and recording over a muscle
- wait for a delayed signal
- has travelled up the nerve to the anterior horn cell then returned to the muscle
F Response
Technique
Supramaximal stimulus is applied to a nerve
- motor nerves are directly depolarised
- like all axons they conduct equally well in all directions
2 impulses
Orthodromic
- which travels to the muscle and produces the typical M response
Antidromic
- which travels back to the anterior horn cell and depolarizes the cell body
- to be detected, the second muscle contraction has to occur after the first has subsided
- only muscles in which the round trip takes over 15 - 20 mS can be used
Problem
Does not measure sensory nerves
Uses
Brachial plexus injury
- want to know if nerve roots intact
- look in muscles relevant for each nerve root
- i.e. stimulate median nerve, look in thenar eminence (T1)
- look to see if F wave intact, delayed or absent
- problem is most muscles supplied by more than one nerve root
Now
- use MRI to see if nerve root avulsion
H Reflex
This is the electrical equivalent of the deep tendon reflex
A mixed peripheral nerve is sub maximally stimulated
- stimulates the large myelinated sensory nerves that convey muscle stretch
- they are the most easily depolarised of the axons
- following a relatively weak stimulus these sensory fibres are selectively depolarised
- a signal ascends to the dorsal root ganglion and then through the monosynaptic reflex arc
- depolarises the anterior horn cells
- causes a secondary signal in the motor axons with a subsequent muscle contraction
Characterised by having a consistent latency
- is elicited by a stimulus so small that it does not cause a direct muscle contraction.
Unfortunately it can only be elicited in the tibial nerve (and recorded over the gastrocnemius)
Electromyography (EMG)
Technique
Needle placed in relevant muscle
- record electrical potential
- at rest and voluntary contraction
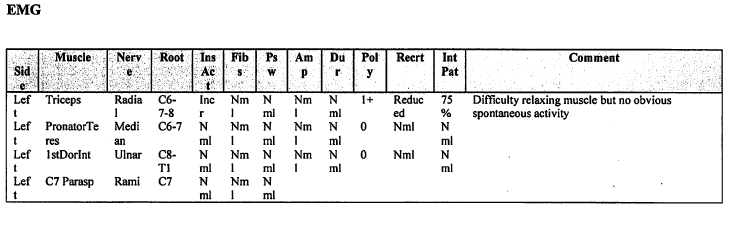
Neuropathy
Denervation
- takes 3/52 to see
- amount of time for wallerian degeneration to occur
- if do earlier will get a false negative
- normal muscle electrically silent at rest
Findings
- spontaneous depolarisation in muscle
- fibrillations
- positive sharp waves
Reinnervation
- takes 3/12 to see
- due to surviving motor axons branching out and recruiting other motor units
Findings
- see large polyphasic motor unit potentials
Myopathy
Muscle problems
- specific patterns of EMG
- Duchenne's muscular dystrophy /myotonica dystrophy
Shortfalls of EMG
It is only a sampling technique
- normal areas in an abnormal muscle may have normal potentials
Specific uses of NCS / EMG
Conduction blocks
SNAP / CMAP
- median nerve, ulna nerve
- confirm entrapment
- evaluate site of entrapment
Axonal / Nerve damage
1. Radial nerve palsy with humeral fractures
Question
- is nerve in continuum or lacerated?
NCS / EMG cannot tell you that
- similar findings for Stage 4 and 5 Sunderland
Can give information regarding severity of injury
- denervation potentials at 3/52
- indicates Sunderland grade 3 or greater
Can give idea of prognosis
- i.e. is there any chance of recovery?
- reinnervation on EMG at 3/12
2. CPN injury at knee, sciatic nerve injury following THR
Can give you idea of prognosis
- i.e. SNAP intact at 3/12
- neuropraxia
Neuropraxia
Minimal axonal damage
- demyelinating / conduction block only
- no Wallerian degeneration
Findings
3/52
- some SNAP and CMAP still seen
- minimal denervation signs i.e. fibrillation
- means nerve is not too badly injured
- prognosis good
- should be just a neuropraxia
Laceration / Neurotmesis
Both conditions will lead to Wallerian degeneration
- severity dependant on number of axons injured
3/52
- no SNAP / CMAP
- may be reduced or no amplitudes depending on number of axons injured
- see fibrillations in muscle in EMG due to denervation
3/12
- looking for reinnervation
- hoping to see large polyphasic AP due to surviving motor axons branching out and recruiting
- if this is not seen, is a poor sign as means no surviving axons
- can repeat later hoping some axons have sprouted down intact tube
Problems with NCS
1. Obese patient
2. Oedema
3. Electrical inteference
- 50 MHz from fluorescent lights
- need to do in Faraday room
- difficult to do in ICU
4. Must remove oils / moisturiser
5. Sweat
Spinal Cord Monitoring
Used to assess spinal cord integrity during spinal instrumentation
Technique
Posterior tibial nerve stimulated
- scalp SEP used to monitor for surgical induced changes
- signal monitored is in the posterior column
- relatively immune to compromise of the anterior spinal artery
- motor control is located anteriorly in the descending corticospinal tracts
