Design


Historical - poor outcomes with cemented implants
3rd generation implants
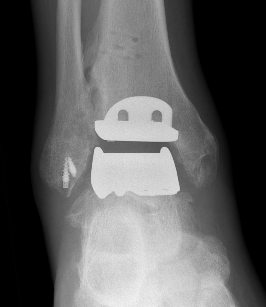
- minimal bony resection with uncemented implants
- talus resurfacing with smooth surface
- +/- stems or pegs
- highly crosslinked polyethelene implant - mobile bearing versus fixed bearing



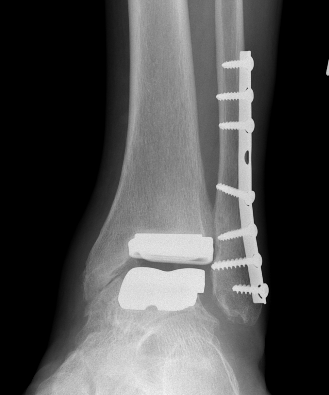
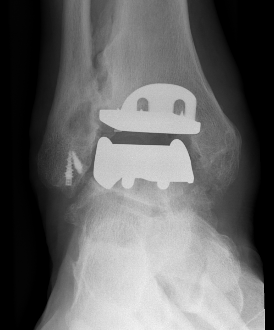
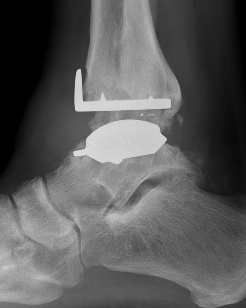
Infinity implant STAR implant Inbone



Agility Salto Tolaris Trabecular metal
Results
10 year revision rate
Australian Joint Registry 2023 Supplementary Report
- 4000 primary TAR
- mean age 65
- 10 year revision rate 15%
3rd and 4th generation implants
Australian Joint Registry 2023 Supplementary Report
- improving outcomes with implants over last 5 years
- prior to 2015: 5 year revision rate: 11%
- since 2015: 5 year revision rate: 6%
Revision rate by prosthesis Australian Joint Registry 2023 Supplementary Report
| Prosthesis | Number implanted | 1 year | 3 year | 5 year | 7 year | 10 year | 14 year |
|---|---|---|---|---|---|---|---|
| STAR | 49 | 4 | 13 | 15 | 22 | ||
| Hintermann | 538 | 4 | 9 | 12 | 16 | 20 | |
| Mobility | 568 | 2 | 7 | 10 | 11 | 15 | 17 |
| Salto | 421 | 2 | 6 | 9 | 12 | 15 | |
| Salto Tolaris | 526 | 1 | 4 | 5 | 5 | ||
| Infinity | 744 | 1 | 3 | ||||
| Trabecular Metal | 339 | 1 | 2 |
Contraindications
| Absolute | Relative |
|---|---|
|
Infection Charcot Poor soft tissue envelope Severe malalignment or instability Talus AVN > 1/3 |
Malalignment Poor bone stock Obesity Diabetes Smoking |
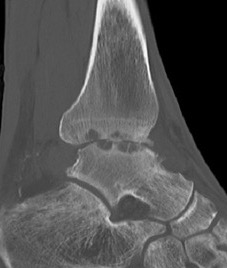
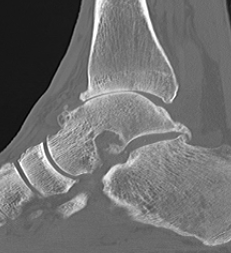
CT
Evaluate bone stock to determine if TAR is appropriate


Technique
A. Anterior approach

Smith & Nephew Salto Tolaris Technique PDF
Vumedi total ankle arthroplasty via anterior approach
Vumedi total ankle arthroplasty with patient specific jigs
Protect SPN and divide extensor retinaculum
- between Tibialis anterior and EHL
- retract neurovascular bundle laterally
- remove anterior osteophytes
Tibial cut
- distal alignment jig / extramedullar jig +/- image intensifier +/- patient specific jigs
- resect few mm above eroded bone
- preserve medial and lateral malleolus
Talar dome resurfacing
- jig to make chamfer cuts
Insert mobile / fixed bearing
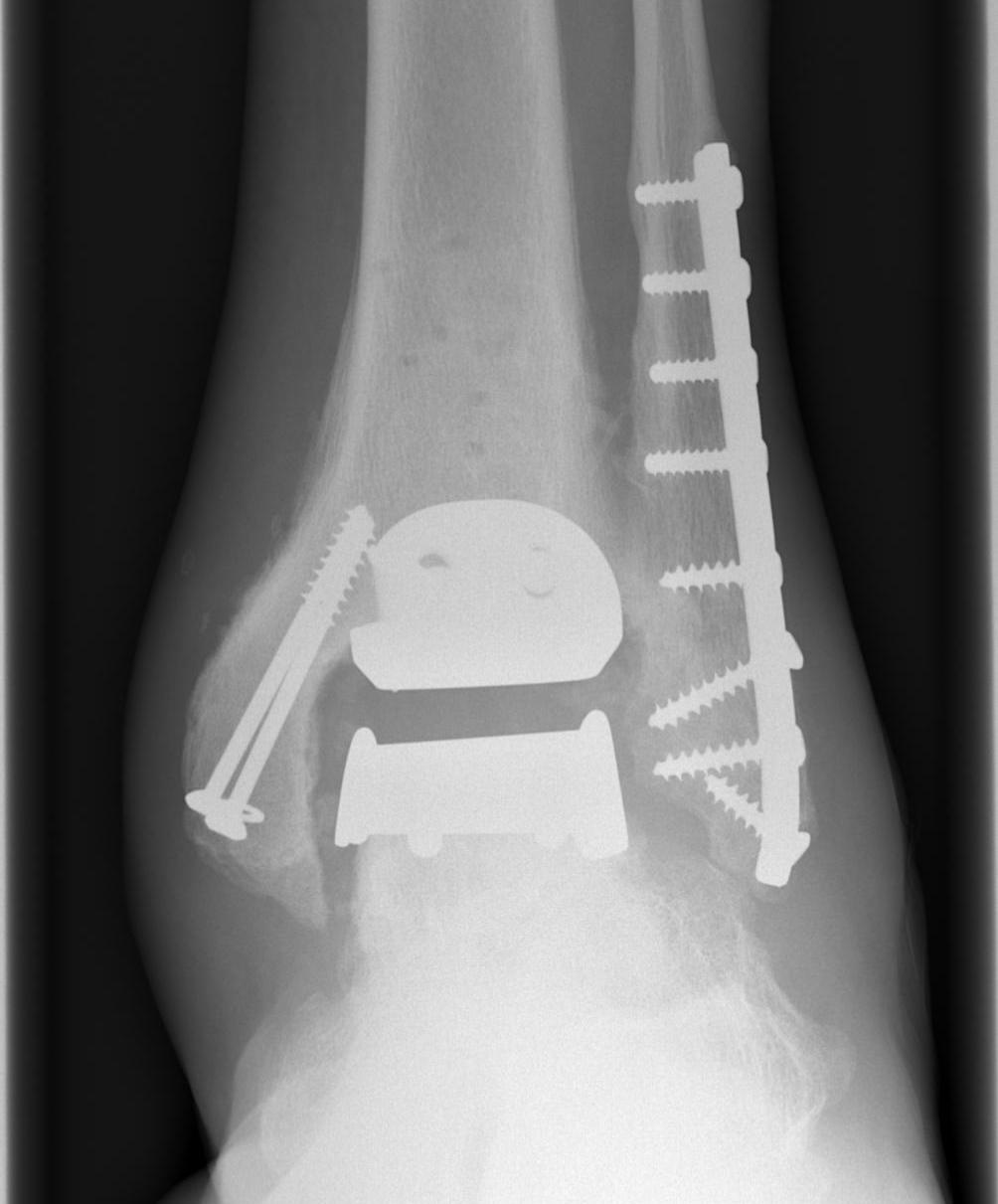
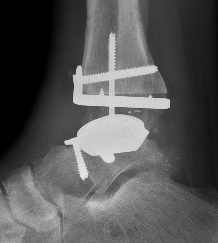
B. Lateral approach and fibular osteotomy

Zimmer Biomet Trabecular Metal PDF
Vumedi fibula osteotomy approach for total ankle arthroplasty
Complications
Australian Joint Registry 2023 Supplementary Report
- 4000 primary TAR
- mean age 65
| Indication for revision | Percentage |
|---|---|
| Loosening | 30% |
| Infection | 13% |
| Lysis | 10% |
| Instability | 9% |
| Implant breakage | 9% |
| Pain | 6% |
| Impingement | 5% |
| Fracture | 5% |
Medial malleolar intra-operative / postoperative fracture


Gutter impingement
Schuberth et al Foot Ankle Int 2013
- incidence of 7% symptomatic gutter impingement
- reduced to 2% if patients underwent prophylactic gutter clearance at time of TAR
- subsequent gutter debridement successful in 80% of patients
Loosening
Options
Athrodesis
Revision TAR
Infection
Acute postoperative
Lachman et al Foot Ankle Int 2018
- 14 acute hematogenous infected TAR
- treated with DAIR and poly exchange
- long term failure rate 54%
Chronic
Conti et al Foot Ankle Int 2022
- 11 patients with chronic TAR infection
- treated with 2 stage revision
- 90% survival at 3 years



2 stage revision chronic infection
Arthrodesis


Revision

Results
Gross et al Foot Ankle Spec 2015
- systematic review of arthrodesis for failed TAR
- 80% union rate
Conversion arthrodesis to arthroplasty
Chu et al J Foot Ankle Surg 2021
- systematic review of conversion arthrodesis to arthroplasty
- 6 studies and 172 ankles
- salvage pantalar fusion 2.3%
- amputation 2.3%