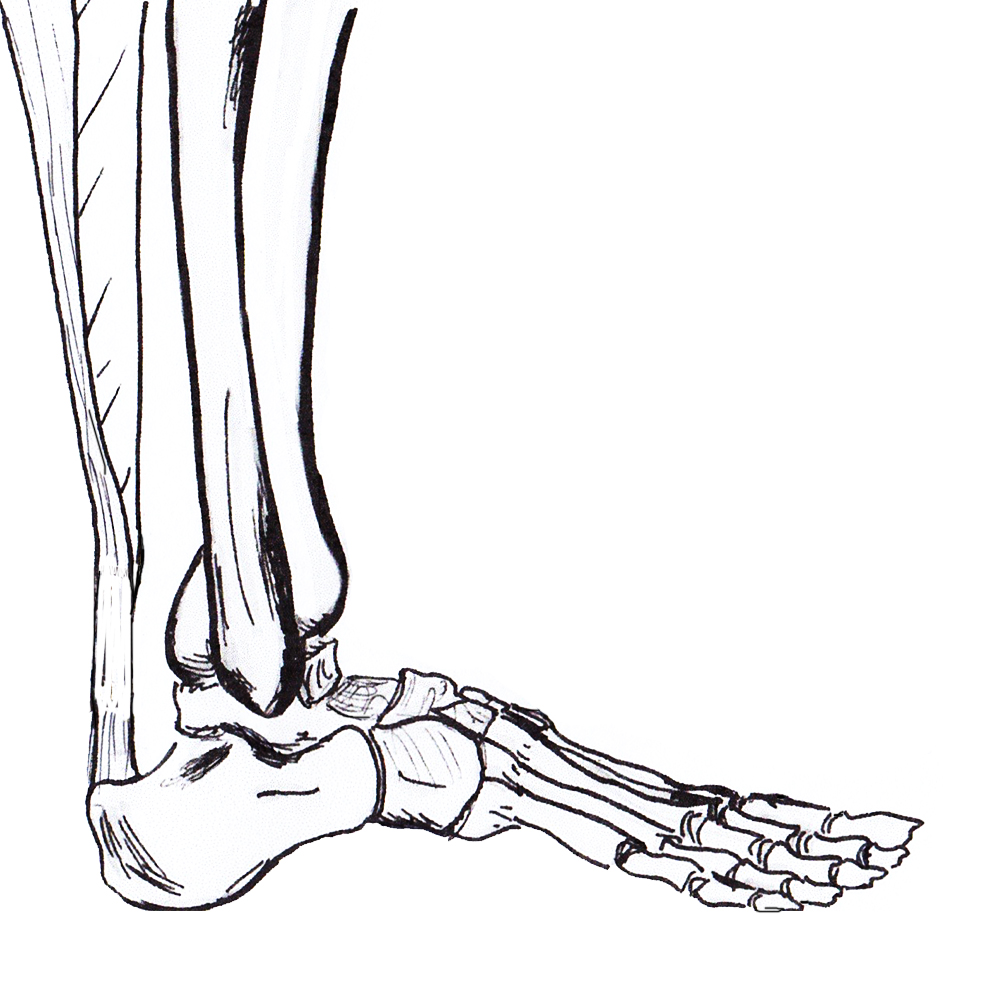
Anatomy
Gastrocneumic and soleus tendon
- longest tendon in human body
- fibres spiral 90° before inserting on superior calcaneal tuberosity
- medial gastrocs inserting posteriorly
- allows elastic recoil & energy storage
Paratenon
- allows smooth tendon movement
Blood supply
- paratenon
- small amount muscle proximally and calcaneum distally
- watershed area 2 - 6 cm proximal to calcaneal tuberosity / area of rupture
Plantaris
- present in 90% population
- medial to Tendo-achilles
Epidemiology
Usually age > 40 years
- M:F = 12:1
- occasional sportsman
- 75% during sports
Etiology
Systematic Factors
- age related changes
- tendonitis
- diabetes / steroid / obesity
- flouroquinolone / ciprofloxacin in elderly
Mechanical Overload / sudden training increase
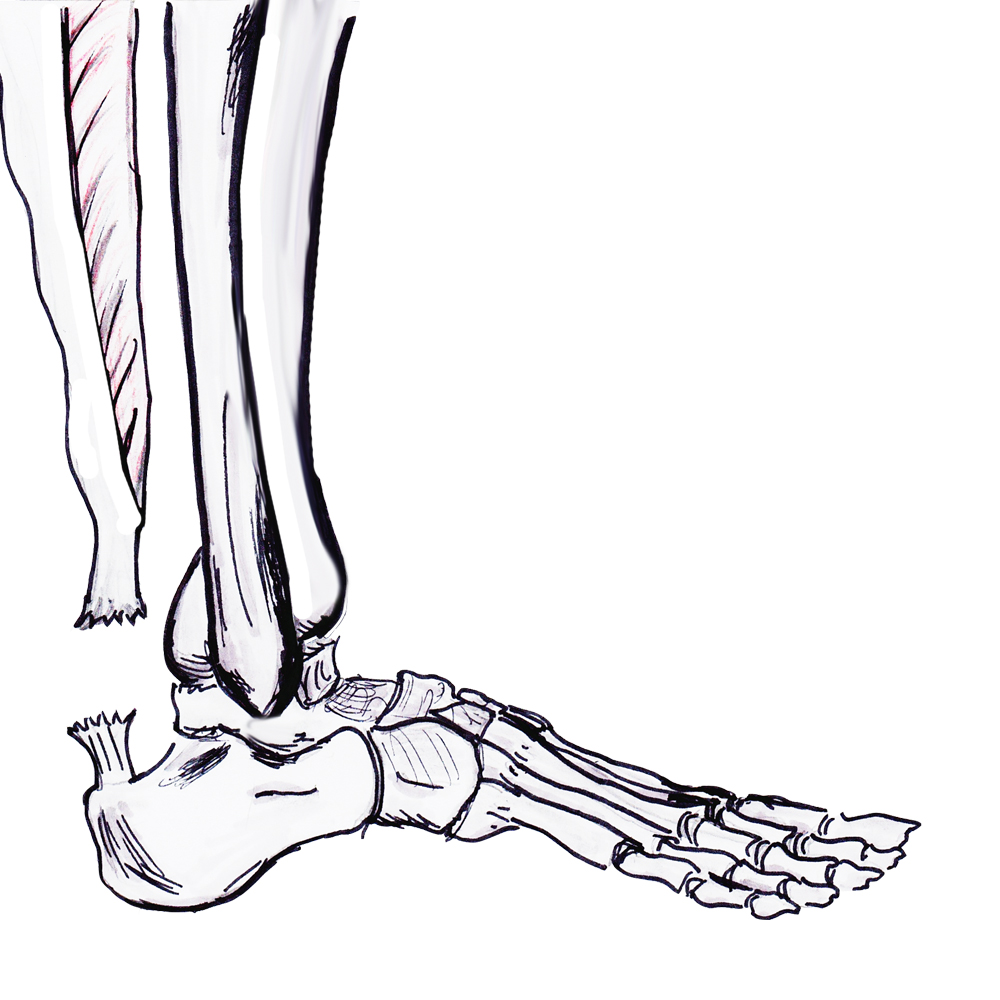
Rupture Site
1. Watershed area
- 5 - 7 cm proximal to insertion
- most common
2. Insertion - insertional tendonitis / diabetes / obestiy
3. Musculotendinous juntion
- avulsion of medial or lateral head
- may present with chronic weakness


Natural history of neglected tears
Weakness / difficulty with push off
- compromised running / jumping / stairs
- can still walk with use of FHL / FDL / T posterior / Peroneals
Symptoms
Sudden pain in calf
Audible snap
Examination
Acute tear


Significant swelling



Visible / palpable gap
Positive Thompson Test
- patient prone
- squeezing calf doesn't produce plantarflexion of ankle
- Thompson test
- sensitivity 0.96, specificity 0.93

Thompson test
Chronic tear
Gap not palpable as gap fills with scar tissue
Excessive dorsiflexion compared with other side

Xray
Exclude bony avulsion / insertional rupture


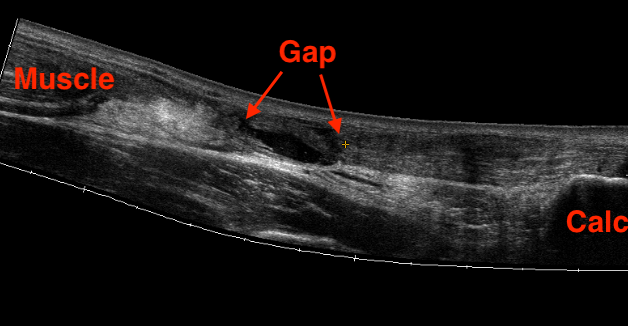
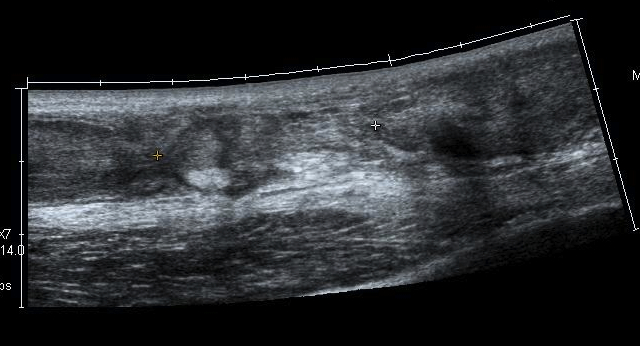
Ultrasound
Diagnose rupture and check reduction of tendon ends with plantarflexion
Aminlari et al J Emerg Med 2021
- systematic review
- ultrasound 95% sensitive and 99% specific for complete rupture
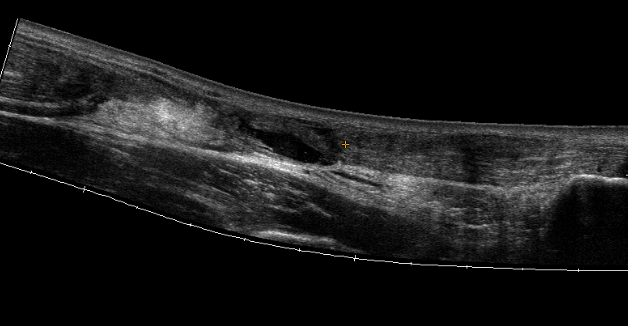
MRI
Indication
- incomplete rupture / clinical uncertainty
- chronic tears - measurement of gap for reconstruction planning
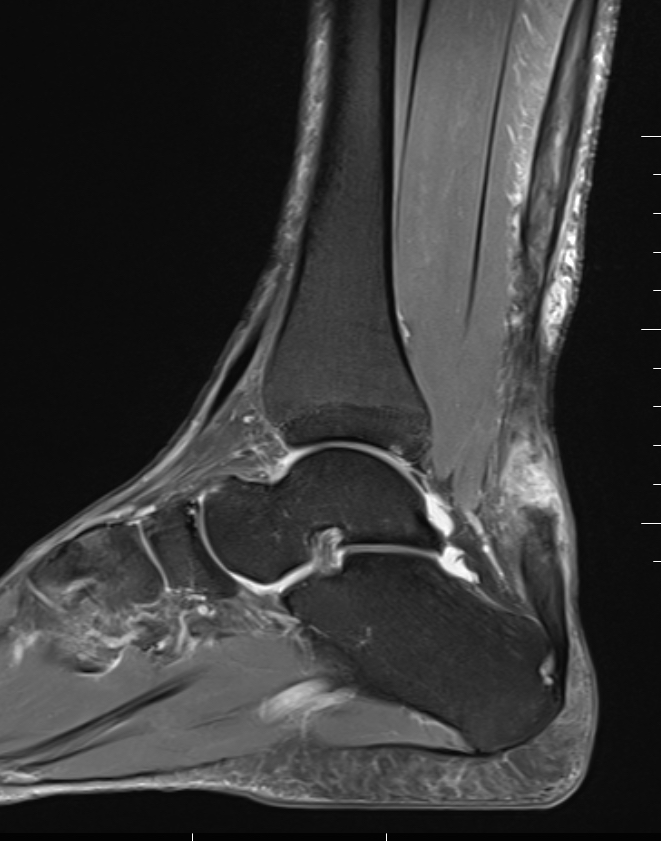

Acute


High grade partial thickness

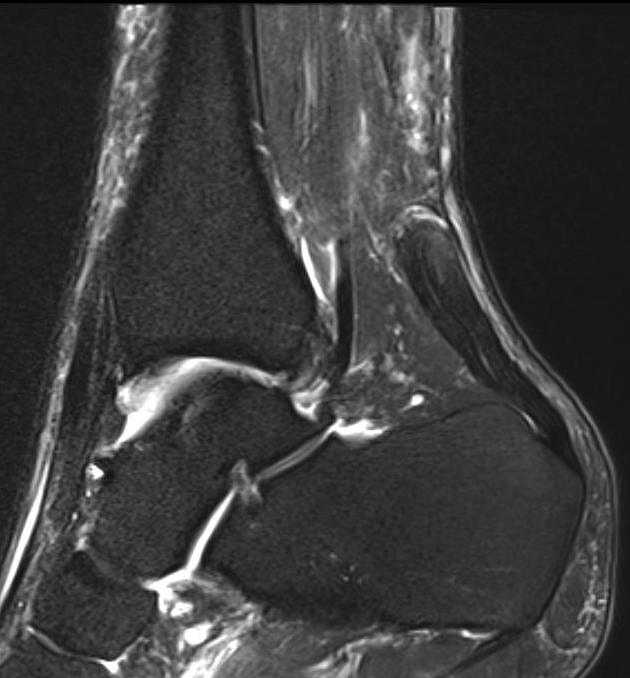

Chronic retracted
Management
Operative v Non-operative Management
Issues
Increased complication rate with operative management
- 1.4% deep infection
- 3% nerve injury
Higher re-rupture rate with non operative management
- 1% versus 6%
Retear
- RCT operative versus nonoperative 526 patients
- no differences between groups in functional outcome
- 6% retear in nonoperative group
- 0.6% retear in operative group
Infection
- meta-analysis of open versus minimally invasive
- superficial infection: open 6%, MIS 0.4%
- deep infection: open 1.4%, MIS 0%
Sural nerve injury
- RCT operative versus nonoperative 526 patients
- 3% nerve injury in open operative group
- 5% nerve injury in the minimally invasive group
Return to sport
- systematic review of elite athletes
- 76% able to RTP, at average 11 months
- those who returned often with decreased performance
- worse than ACL injuries
Zellers et al Br J Sports Med 2016
- systematic review of 6,500 patients
- return to sports 80%
Bak et al J Foot Ankle Surg 2024
- systematic review
- no difference return to sports between operative and nonoperative
Non-operative management
Technique
Functional rehabilitation
A. 2 weeks equinus front slab within 24 hours
- close gap before haematoma forms
B. 2 - 8 weeks full weight bear in air cast with heel raise 2 cm
- active ROM below neutral

Results
Dai et al J Sci Med Sport 2021
- systematic review of non operative management
- immobilization versus early functional rehabilitation
- no difference in functional outcome / rerupture / return to sport
- safe to early mobilize and weight bear in brace
Operative
Indications
Athlete
Delayed initial treatment
Wish to reduce retear rate
Options
Open
Minimally invasive
- meta-analysis of open versus minimally invasive
- 10 RCTs and 500 patients
- no difference functional outcome
- rerupture rate: open 2.5%, MIS 1.5% (not significant)
- sural nerve injury: open 0%, MIS 3.4% (significant)
- superficial infection: open 6%, MIS 0.4% (significant)
- deep infection: open 1.4%, MIS 0% (not significant)
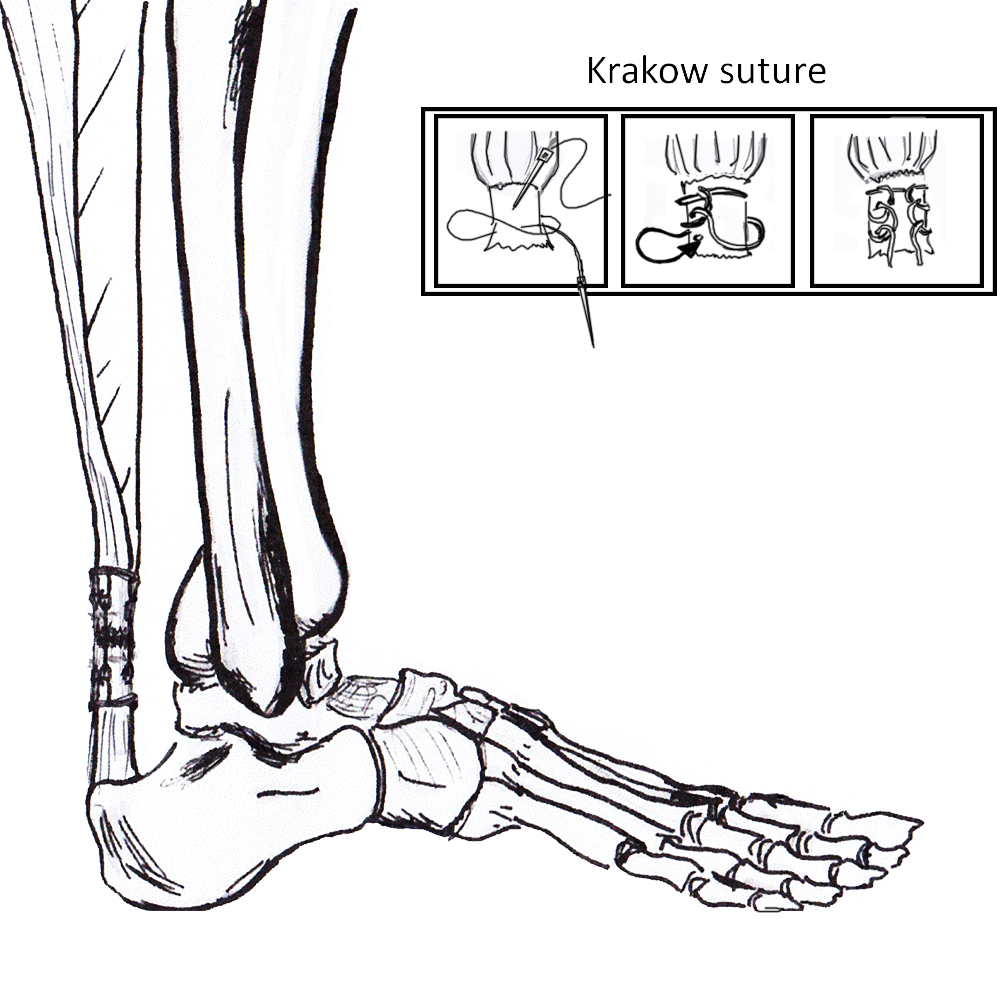
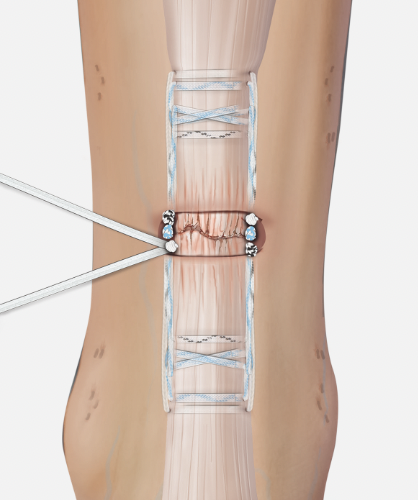
Open tendoachilles repair
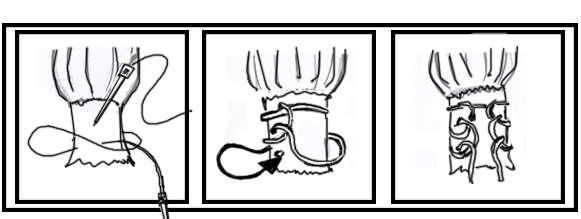
Technique
Vumedi open achilles tendon repair
Prone position with tourniquet
- slightly medial incision to protect sural nerve
- full thickness skin flaps to paratenon
- identify and protect sural nerve
- divide paratenon longitudinally
- can incise paratenon in the midline anteriorly which increases tissue available for closure
- Bunnell Suture / Krackow suture x 2 with high strength suture / fibre wire
- one in proximal and one in distal tendon ends
- tie via two knots with foot fully plantar flexed
- +/- augment with circumferential 4.0 suture to minimize bunching
- careful closure of paratenon to prevent skin adhesions
- front slab in plantarflexion 2 weeks
- then standard accelerated rehabilitation

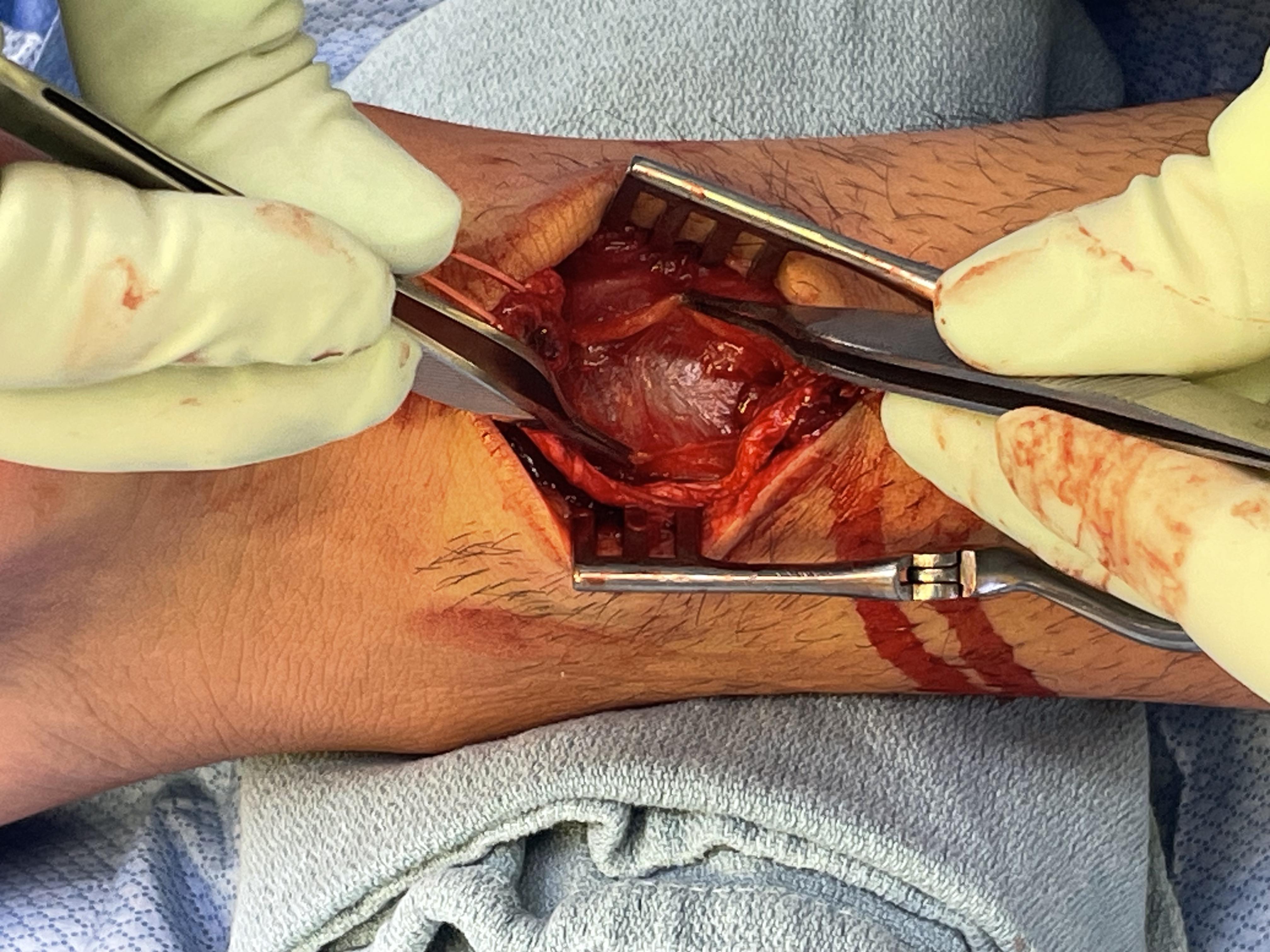
Anterior release of paratenon to allow posterior closure over achilles repair
Repair with proximal and distal Krackow high strength sutures
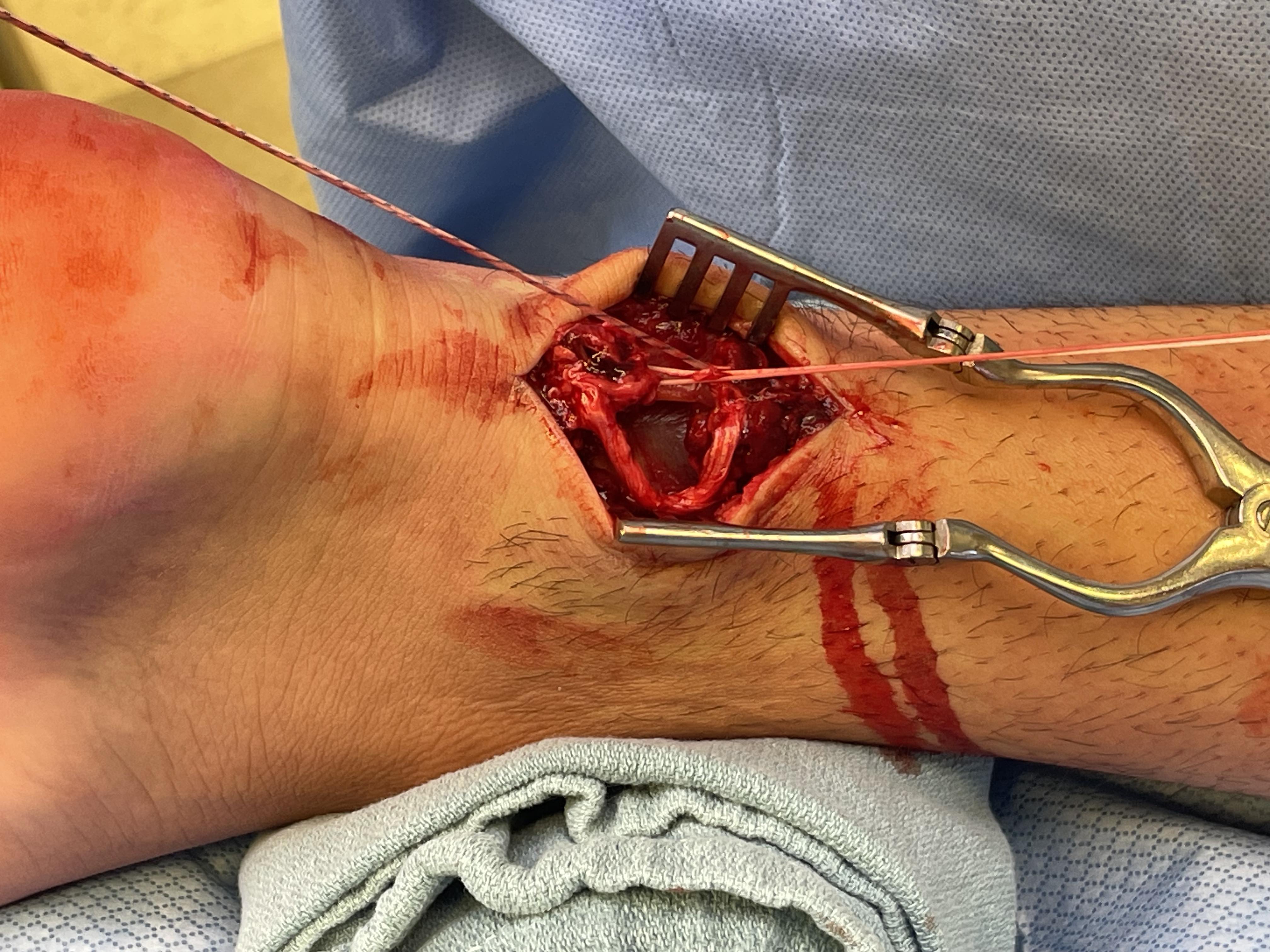
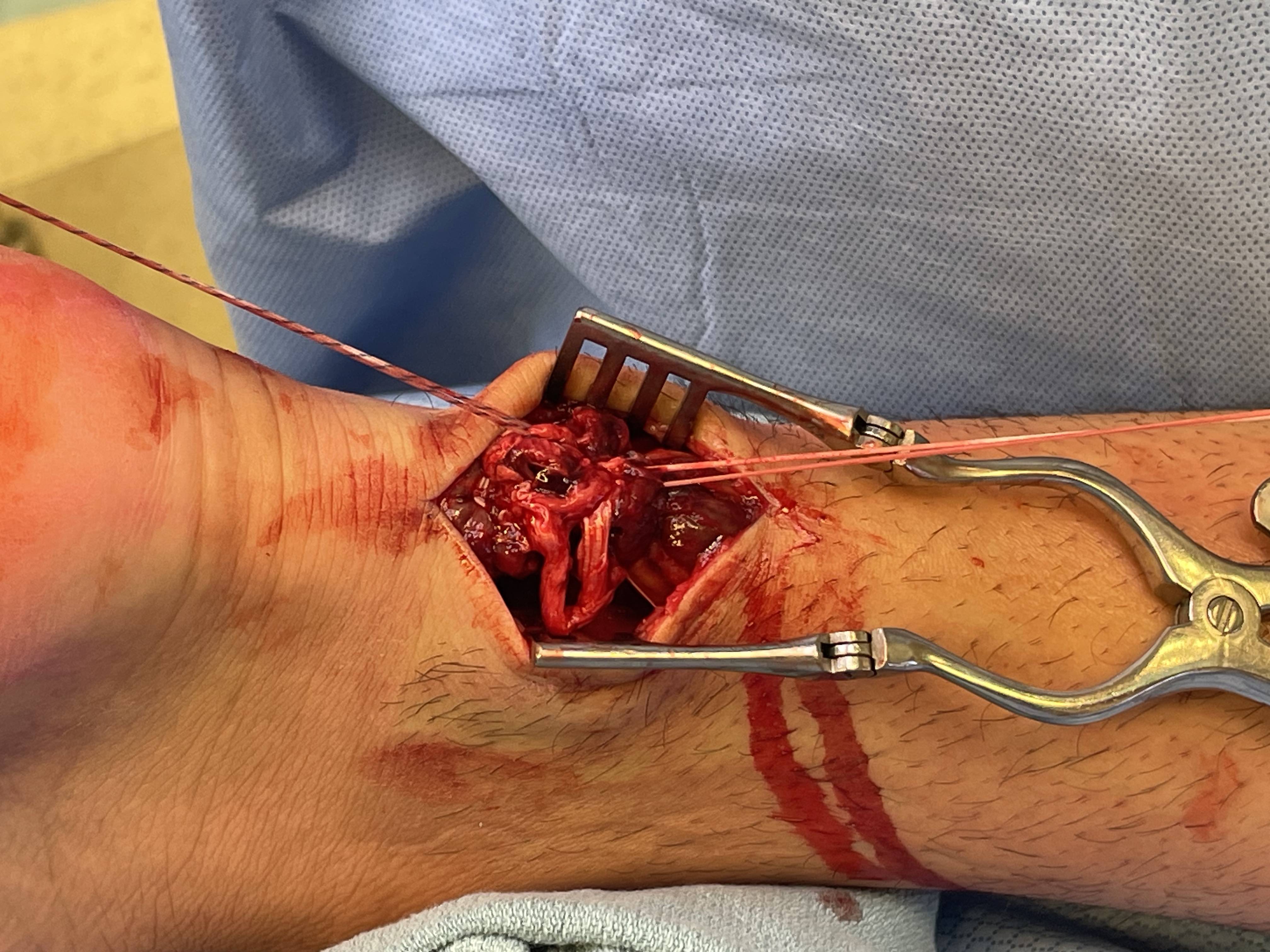
Minimally invasive repair
Percutaneous suture technique
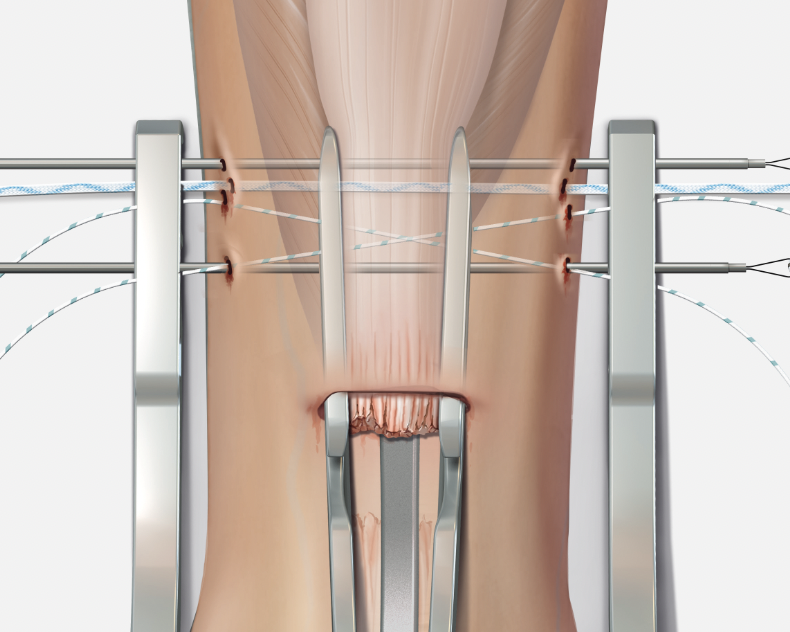
Arthrex PARS
Vumedi percutaneous repair video
Calcaneal anchor technique
Arthrex Speedbridge technique
Vumedi Arthrex Speedbridge in calcaneum
Vumedi stryker anchors in calcaneum video
Rehabilitation
- systematic review of rehabilitation after operative repair
- lower complications and better outcomes with early weight bearing and ankle ROM exercises
Complications
Infection / wound breakdown


Wound breakdown
- free muscle flap + split skin graft
- fasciocutanous flap (radial or lateral thigh)
DVT / PE
Blanco et al J Foot Ankle Surg 2018
- prospective cohort and 90 incidence of DVT / PE
- achilles tendon in cast: 5%
- ankle fracture cast / no surgery:2%
- ankle fracture surgery: 3%
Rerupture



New incomplete tear seen on MRI

Rerupture with scar tissue between tendon ends
Reconstruction
Algorithm
| Defect | Method |
|---|---|
| < 3 cm | Turndown |
| 3 - 5 cm | V-Y lengthening |
| > 5 cm |
Local tendon graft - FHL / Peroneus brevis Free tendon graft |
Turndown
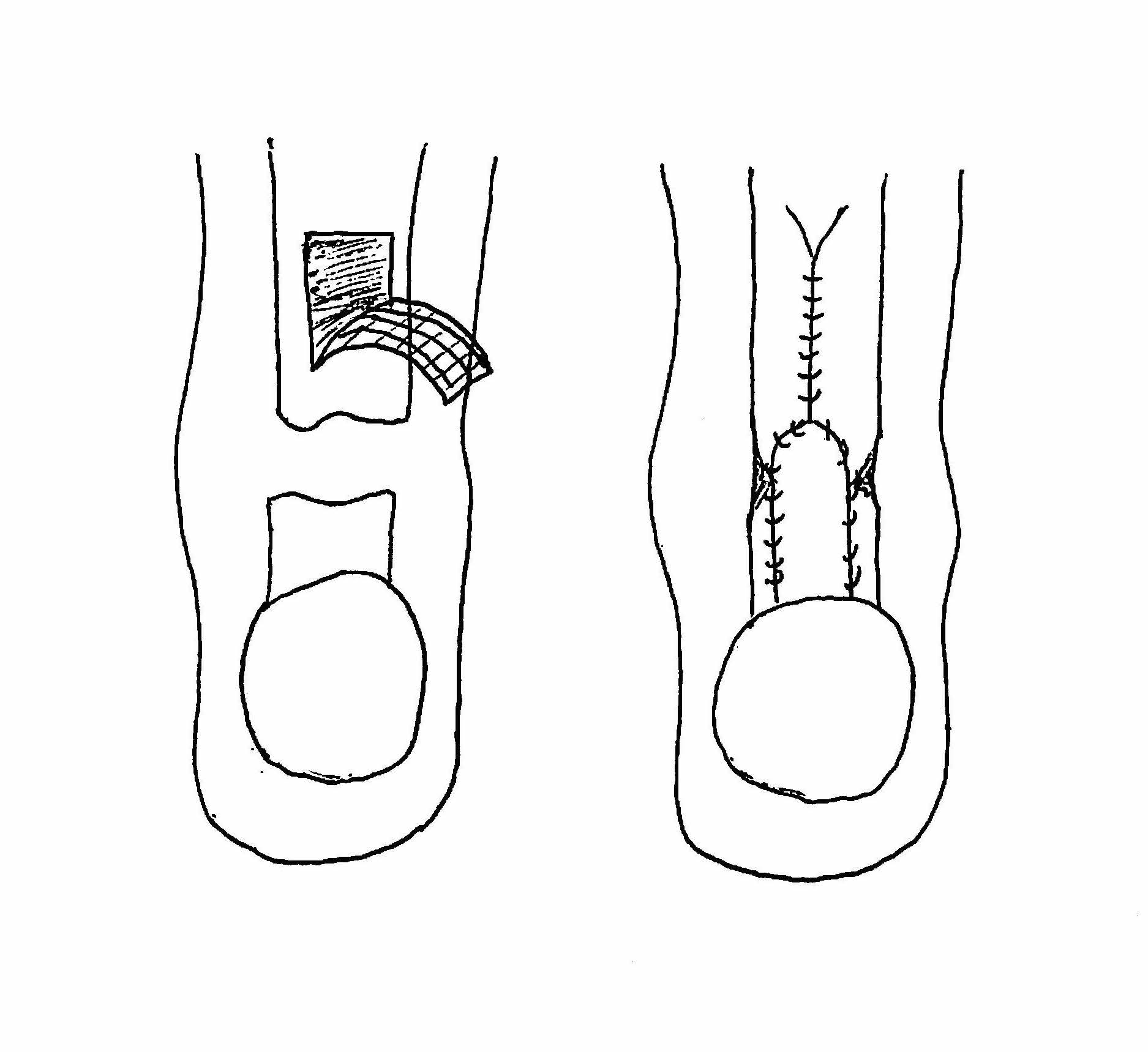
Technique
Bosworth technique
- harvest central third fascia
- from musculotendinus junction as far proximal as possible
- leave attached distally, detach proximally
- closure fascia above
- tubularise fascia with 2.0 ethibond
- drill hole through calcaneal tuberosity
- pass through calcaneum
- suture to itself
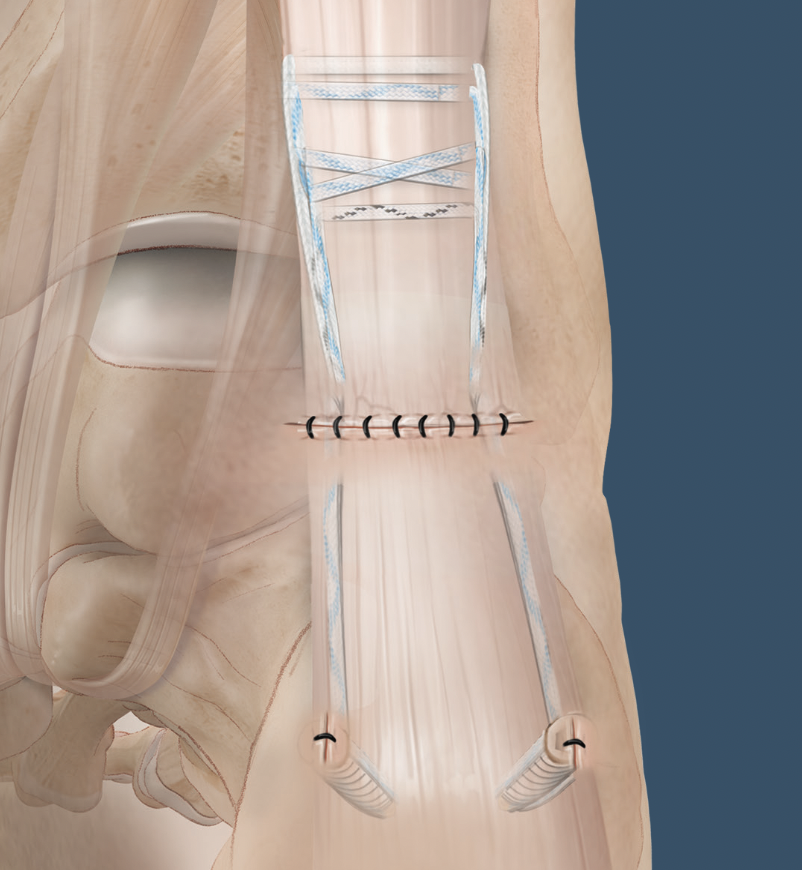
VY lengthening
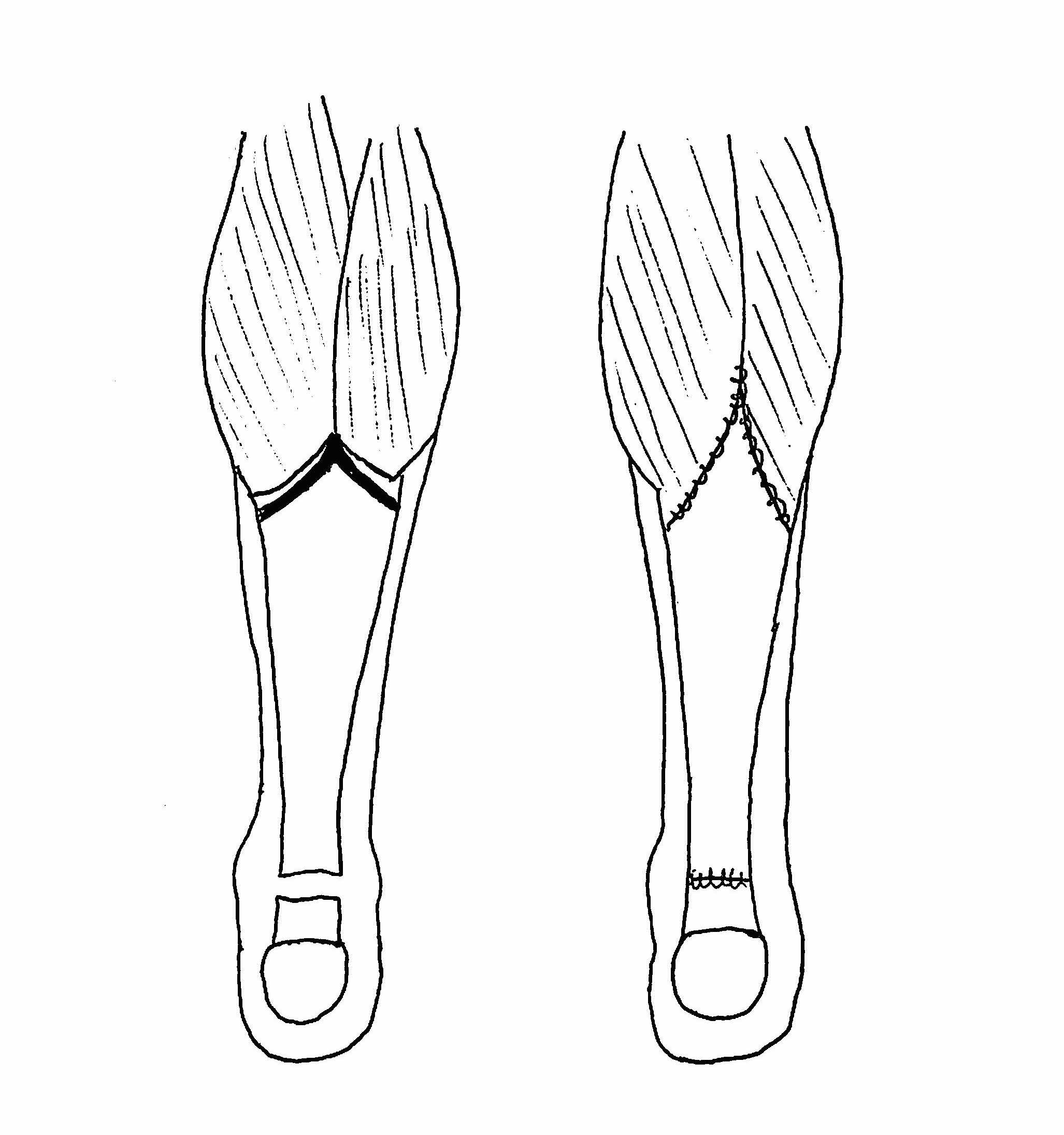

Technique
Vumedi VY lengthening + FHL transfer video
Local tendon grafts
Options
FHL
Peroneus brevis
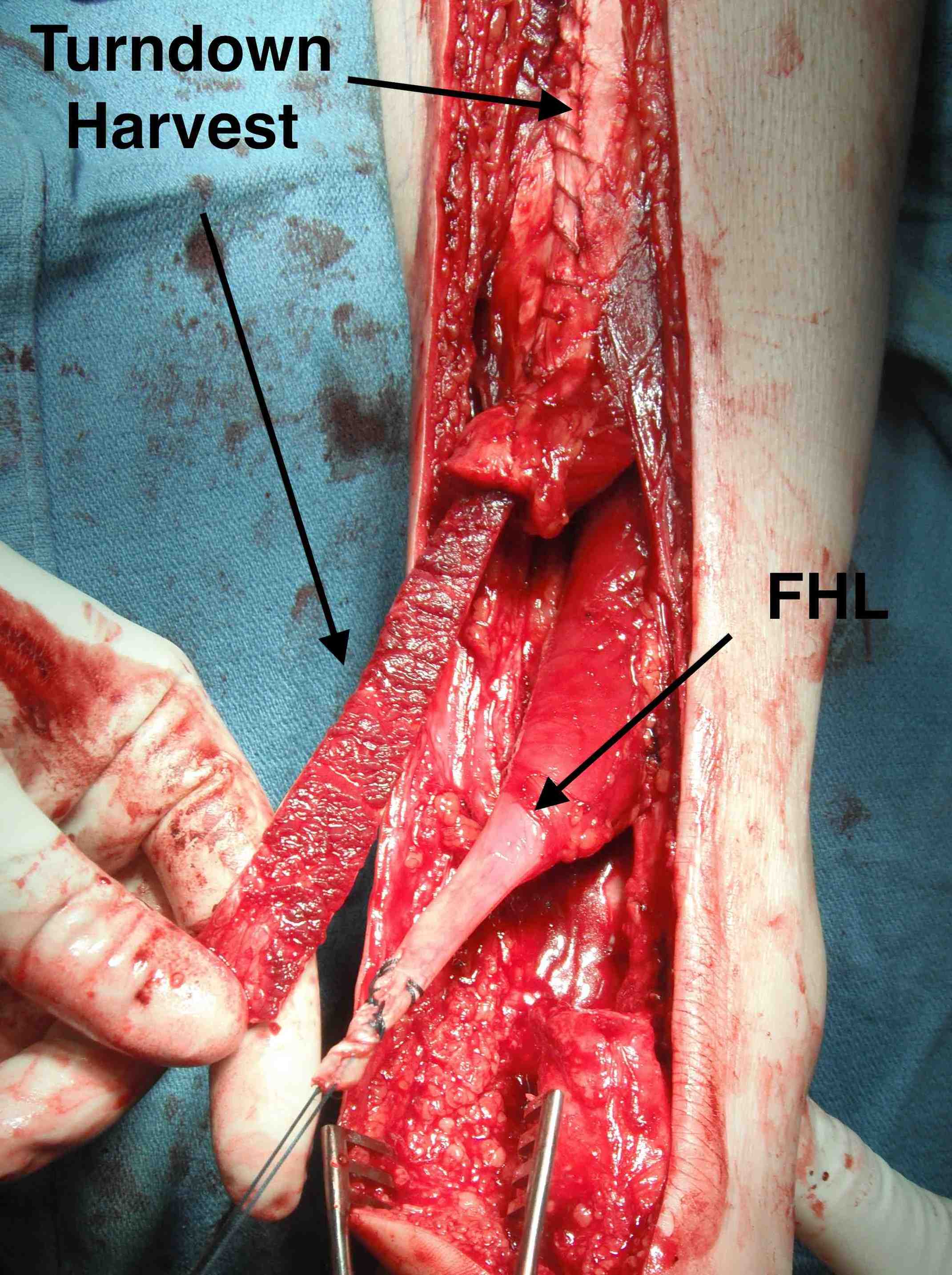
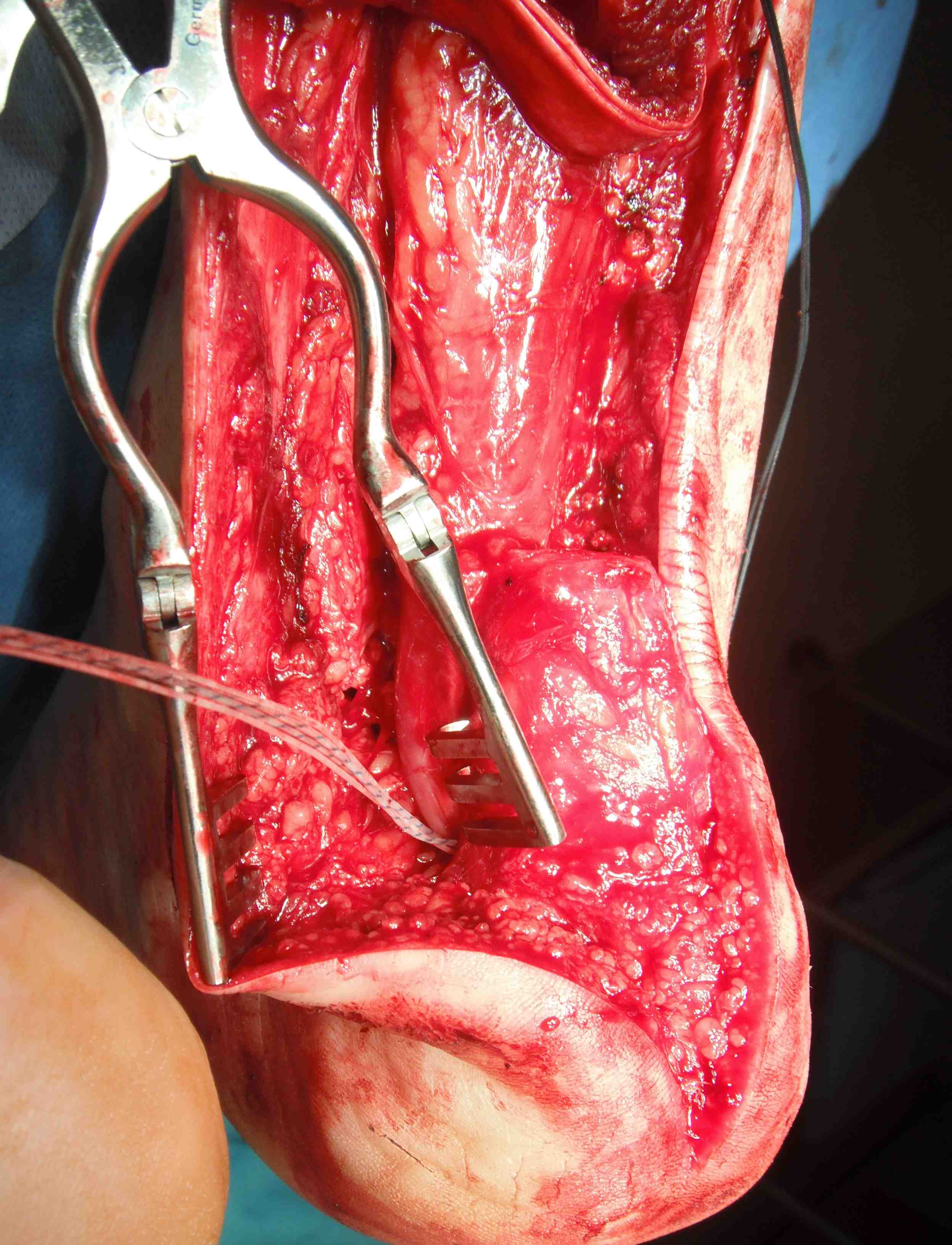

Turndown + FHL transfer with FHL passed through a transverse tunnel in the calcaneum
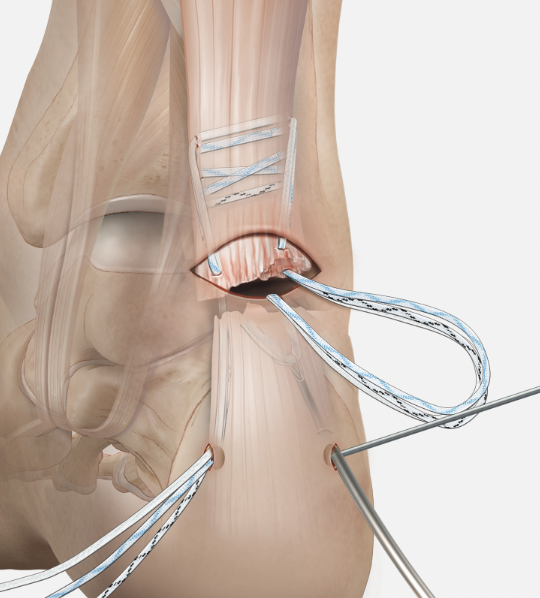
FHL transfer
Technique
Vumedi VY lengthening + FHL transfer video 1
Vumedi VY lengthening + FHL transfer video 2
Identify FHL tendon medially
- identify and protect tibial nerve
- pull tendon through and transect with sufficient length
- through drill hole in calcaneum and secure
Peroneus brevis transfer
Technique
Identify peroneus brevis tendon laterally
- small incision over base 5th metatarsal
- divide tendon
- pass through calcaneal drill hole and secure
Results
Maffulli et al J Clin Med 2023
- systematic review of local tendon grafts for achilles reconstruction
- 79% able to return to previous activity
Free tendon grafts

- systematic review of chronic tears with > 6 cm
- free tendon grafts
- 22 articles and 400 patients
- 80% no activity limitations
- 50% return to sport