Portals
1. Anterolateral
Viewing portal
- 1cm lateral to patella tendon
- 1cm above joint line
- 1 cm below inferior pole patella
Problems
- too medial, in fat pad
- too high, limitation by patella, difficult to see posterior horns
- too low, damage anterior horn meniscus
Limitations
- PCL
- anterior horn LM
- posterior horn MM in tight knees
2. Anteromedial
Instrumentation portal
- also used for viewing posterior horn MM, anterior horn LM
- 1 cm above joint line
- 1 cm lateral to patella tendon
- 1 cm below inferior pole patella
Can be useul to insert needle first
3. Superolateral portal
Landmarks
- just lateral to quadriceps tendon
- 2.5 cm above SL corner of patella
Uses
- evaluate PFJ
- drainage portal
- resection plicae
- removal loose bodies
4. Posteromedial portal
Must
1. Have distended the knee with saline so the soft spot bulges
2. Flex the knee to 90o so NV bundle falls posteriorly
3. Marked the bony landmarks prior
Landmarks
- 1 cm above joint line
- 1 cm posterior to MFC
- flex knee slightly
- introduce needle & then skin incision and blunt dissect to post capsule
- pass switching stick / insert cannula over it
Anatomical
- anterior to medial head gastrocnemius
- posterior to MCL / MFC
- superior to pes
Uses
- posterior horn tears MM
- loose bodies
- PCL reconstruction / posterior tibial joint line debridement
Risks
- saphenous nerve
5. Posterolateral Portal
Technique
- distend joint with fluid
- knee at 90o
Landmarks
- where posterior margin of femoral cortex intersects posterior aspect of fibula
- 2cm above joint line
- behind LFC
Anatomy
- behind LCL
- anterior to lateral head gastrocnemius
- between ITB and biceps
Uses
- repair posterior lateral meniscus
Risks
- CPN
6. Accessory far medial and lateral portals
2.5 cm medial and lateral to standard anterior portals
Uses
Far medial portal
- gives good access to body of lateral meniscu
- angle is above the tibial spines
7. Central trans-patella portal
Landmarks
- midline
- 1cm below inferior pole patella
Uses
- ACL
- OCD
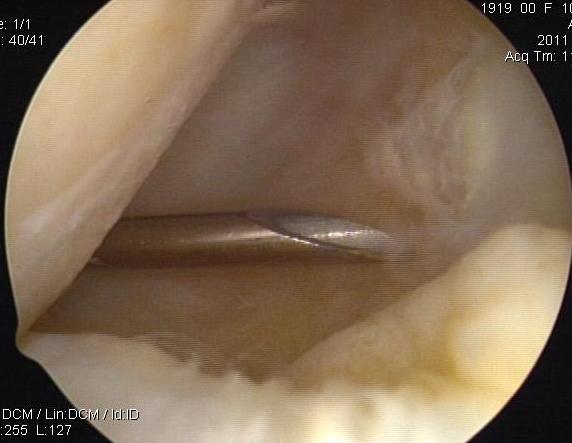
8. Trans-septal portal
Surgical technique PDF using trans-septal portal
Incisions for Inside / Out Sutures or Removal of Loose Bodies
Posteromedial incision
Placed at the posterior aspect of MFC
- knee in 90° flexion
- 3-4 cm long
- 1/3 of incision above joint line & 2/3 below
- medial head gastrocnemius posterior
- MCL anterior
- infrapatellar branch of saphenous nerve 1 cm above joint line
- avoid saphenous nerve which runs in fat above the sartorius
- open sartorius fascia, retract to protect nerve
- expose capsule
Posterolateral incision
Centred on joint line
- knee at 90o
- LCL
- biceps inferiorly to protect CPN
- must dissect lateral gastronemius off capsule and retract
- protects posterior neurovascular bundle
Complications
Incidence
Uncommon
- overall < 1%
- NV complications rare
- incidence 0.1%
Nerve Injury
From incorrect placement of portals
Risk reduced by
- correct placement
- use of blunt trocar
1. Infrapatellar branch saphenous nerve
- anteromedial portal
2. Saphenous Nerve
- most commonly injured
- usually from posteromedial portal
- needles during arthroscopic in-out meniscal repair
3. Common Peroneal Nerve
- second most commonly injured
- direct puncture for posterolateral portal
- passage of needles for arthroscopic meniscal repair
- entrapment by sutures of meniscal repair
Can be avoided by
- flexion of knee
- direct dissection & identification
- use retractor to deflect needles
Tourniquet related Neuropraxia
Risk reduced by
1. Minimal duration
- < 90 min UL
- < 120 min LL
2. Minimal pressure
- < 250 UL
- < 350 LL
3. Adequate cuff width
- > 1.2 limb diameter
4. Positioning
- direct pressure on nerve from inappropriate positioning
RSD
Uncommon
Considered when
- prolonged pain > than expected
- vasomotor disturbance
- stiffness
- trophic changes
Compartment Syndrome
From extravasation of fluid for distension of joint
- fluid may enter through rupture of synovial pouch
- into thigh through suprapatellar pouch
- into calf through semimembranosus bursa
Risk reduced by
- minimise water pressure used
- minimise duration of procedure
- absorbable solution
- minimise number of capsular punctures
- avoid 6/52 post injury
- palpate leg at end of procedure

Management
- usually will resolve
1. Keep patient asleep
- elevate foot
- compress with eshmarc bandage to remove water
2. Mini incision in fascia
- allows water to escape
- will see muscle is very oedematous
3. Ensure patient has not had vascular injury
