Aim
Establish normal biomechanical forces about the hip
Decision Making
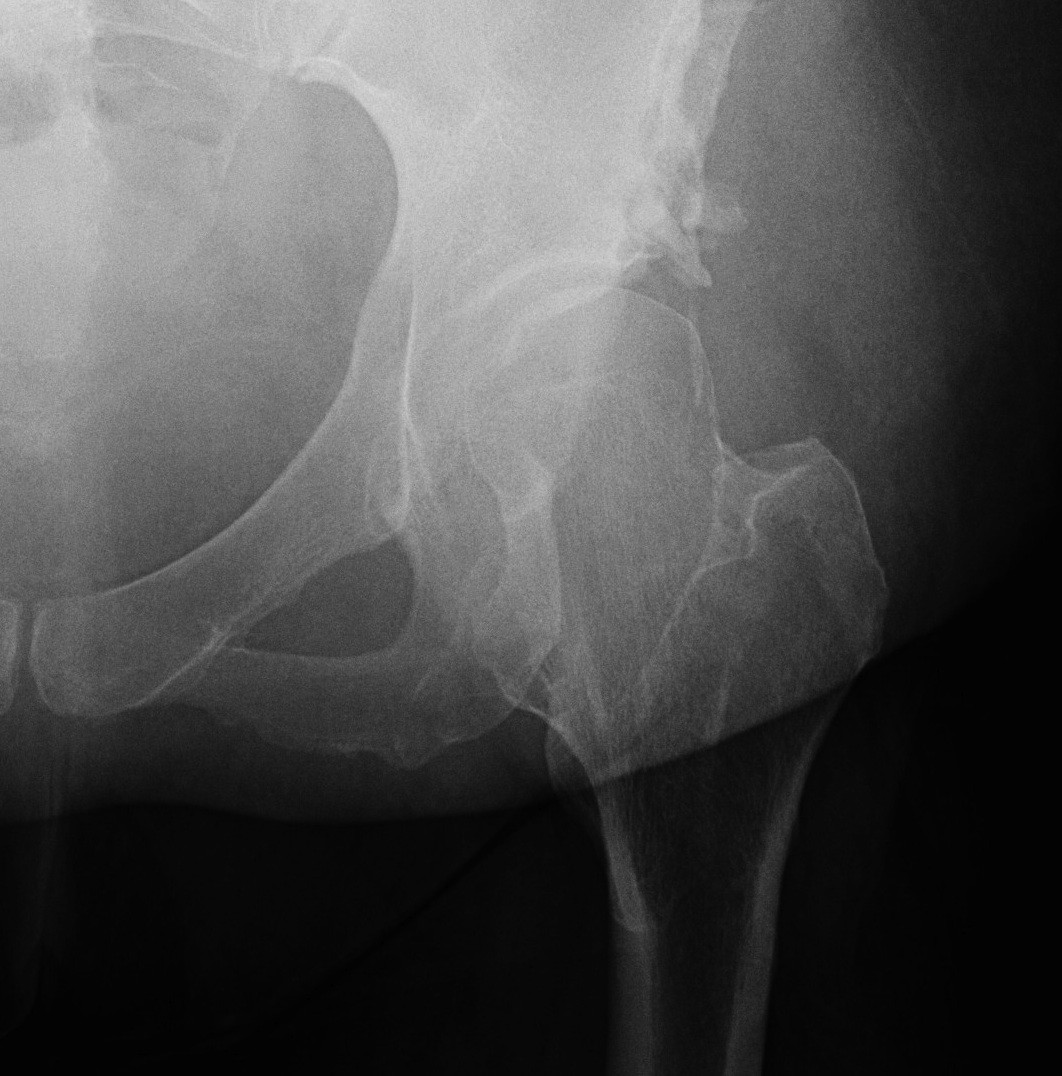
1. Will the hip remodel? - < 8 years old
2. Can congruency be obtained?
3. How much correction is required?
Types of Pelvic Osteotomies
1. Reconstructive Osteotomy
- redirectional
- reshaping
2. Salvage Osteotomy
Reconstructive Osteotomy
Best option for the young patient with symptomatic acetabular dysplasia
- i.e. AI > 40o and CE < 20o with mild OA
Indications
- AI > 40o
- CE < 20o
- symptomatic dysplasia
- congruent joint
- spherical head
- preserved articular space (relative) / mild OA
- minimum 70° flexion / extension arc
- subluxation can be reduced
A. Redirectional
Single osteotomy - Salter
Double osteotomy - Sutherland
Triple - Steele / Tonnis / O'Hara Interlocking Modification
Periacetabular Osteotomy - PAO / Bernese / Ganz
B. Reshaping
Pemberton / Dega
Salvage Osteotomies
Indication
If the OA is too severe for a reconstructive osteotomy
In the age of modern THR
- THR is probably a more reproducible option than a salvage osteotomy
Options
Shelf /Staheli / Melbourne
Chiari
Specific Osteotomies
1. Salter
Concepts
- single osteotomy / innominate
- can do in older patient but difficult unless experienced with operation
- relies on motion at symphysis pubis to rotate acetabulum
Indications
- can't do bilateral Salters
- mild to moderate dysplasia / DDH
- concentric reduction
- near normal ROM
- no OA
- undeformed head
Advantage
- correct CE 10o
Disadvantage
- add 1 cm LL
- leave deficient posteriorly
Results
Salter CORR 1974
- 53 adults 4 year followup
- increased CEA by average 18°
- decreased AI average 50° to 38°
- 63% no pain / 40% no limp (compared with all patients preop)
- 79% trendelenburg negative (compared with 96% positive preop)
Technique
Supine
Smith Petersen approach
- anterior 2/3 crest
- 5cm below ASIS
- between TFL and Sartorius
- protect LFCN medially
- tie ascending branch LCFA
- between G medius and R femoris
- clear glutei and iliacus off pelvis
Right angle about G Sciatic notch
- protect SGN and SGA
- gigli initially in notch
- anterior saw blade above acetabulum between AIIS and ASIS
Leg in figure 4
- rotate acetabulum anterolaterally through symphysis pubis
- x-ray shows narrowing of obturator foramen
- 30o iliac wedge crest
- fix with threaded K wires
- protect for 6 / 52
2. Sutherland
Concept
- double osteotomy
- Salter plus osteotomy lateral to pubic symphysis
Disadvantage
- can be difficult to move because osteotomy further away from acetabulum
3. Steele
Concept
- triple / innominate osteotomy
- salter with two pubic osteotomies
- similar to Tonnis but ostetomies are a bit further away from acetabulum
Indications
- for older child with less mobile pubic symphysis
Technique
- osteotomy at base of ischial rami via posterior approach
- osteotomy superior pubic rami
Advantage
- allows more correction whilst not laterally displacing the joint as a Salter tends to do
- can improve CE 20o
4. Tonnis
Concept
- Salter osteotomy plus pubis and ischial between ischial tuberosity and acetabulum
- get better or easier correction because osteotomies are closer to acetabulum
5. Ganz
Concept
- periacetabular osteotomy
- posterior column left intact for stability
Indications
- older adolescent and adults
- with residual dysplasia
Advantage
- excellent rotation with medialisation
- increase CE 27o
Technique
- isolate acetabulum from ileum / ischium via 3 part osteotomy
- separate superior rami osteotomy at base
6. Dial
Concept
- curved osteotomy following periphery of acetabulum
- don't see sciatic nerve
- a lot of operation is done by feel
Disadvantage
- risk of acetabular AVN and fracture
- technically very difficult
7. Pemberton
Concept
- incomplete transiliac osteotomy
- cut into iliopubic and ilioischial limbs triradiate cartilage
- bends through triradiate cartilage
Indications
- only in those < 8 with open triradiate cartilage
Advantage
- decreases volume of acetabulum
- provides very good cover
Disadvantage
- may sublux the hip after reduction so always check
8. Dega
Concept
- incomplete trans-iliac osteotomy
- rely on plasticity of superior acetabular margin rather than triradiate
Advantage
- excellent reduction of AI
- improvement CE average 31o
- very stable
Technique
- anterior approach
- osteotomy sites 15 mm from articular surface
- hip capsule not violated
- anterior and middle portions ileum cut
- leave posterior wall and G sciatic notch intact
- directed downwards
9. Shelf


Indications
- older child > 12 years
- congruent reduction impossible
Concept
- extra-articular bony buttress over uncovered anterolateral portion of femoral head
- iliac wing graft placed over hip capsule
- place graft under reflected head of RF
- can be modified depending on where cover is needed
Disadvantage
- if not weight bearing (i.e. too high) will undergo resorption
- if too low, will cause pain
Stahelli Technique
- take off reflected head of rectus
- supra-acetabular slot, matchstick corticocancellous iliac graft
- graft strips are placed into slot which is checked radiographically to ensure as low as possible
- rectus tied over the top
- pack morselised graft over the top
10. Chiari
Concept
- medial displacement to develop shelf
- cartilage interposed to develop fibrocartilage
Results
Luiket al JBJS 1991
- 82 of Chiari's original patients
- 20 required THR
- 75% good
- best results: 80% coverage, < 45 years, high osteotomy slope, adequate medialisation
Reynolds JBJS 1986
- 90% success at 5 years
Pitfalls
1. Distal fragment must go medially & adducted
2. Must angle osteotomy anterolaterally distally to posteromedial proximally
3. Anterior defect needs bone grafting
Specific Indications
DDH
Dislocation / 18 months
- Salter
- Dega
- Pemberton
Residual Dysplasia
Before Maturity
- Salter (through pubis)
- Dega
- Pemberton (through triradiate)
After Maturity
- Tonnis
- PAO i.e. Ganz
Salvage
- Chiari / Shelf
Perthes
- Salter
- Triple
- Shelf
CP / Neuromuscular
- Dega / Triple
- Shelf / Chiari
