Management Principles
Stage the infection, the host & the management
1. Stage host / maximise healing potential
2. Stage infection / MCS / sensitivities
3. Debride all infected bone and ST
4. Stabilise skeleton
5. Eliminate dead space
6. Soft tissue coverage
7. Eradicate infection
8. Deal with bone loss / obtain union
Aetiology
1. Secondary to acute osteomyelitis
2. Post traumatic
- usually following open fracture
- tibia most common
3. Post operative
- usually after implantation of prosthesis
- ORIF, total joint replacement
Cierny Classification
Anatomic
Host
Clinical
1. Anatomic
Type 1 / Medullary Osteomyelitis
- nidus is endosteal
Type 2 / Superficial Osteomyelitis
- secondary soft tissue breakdown
- infected cortex due to soft tissue defect
Type 3 / Localised Cortical & Medullary Osteomyelitis
- well marginated sequestration of cortical bone
- entire lesion can be excised without causing instability
Type 4 / Diffuse Cortical & Medullary Osteomyelitis
- involves entire segment bone
- unstable pre or post debridement
- infected non union
2. Host
Type A / Healthy
- good systemic defences
- good local vascularity and a normal physiologic response to infection and surgery
Type B / Compromised
- either local, systemic, or combined deficiency in wound healing and infection response
Type C / Not a surgical candidate
- requires suppressive or no treatment
- has minimal disability
- or for whom the treatment or results of treatment are more compromising than the disability caused by the disease itself
3. Clinical
I Simple dead space & simple closure
II No dead space & complex closure
III Simple stabilisations with complex dead space & closure
IV Complex stabilisations / closure / dead space
Pathology
1. Bone erosion
2. Cortical & subperiosteal new bone formation
- cavities containing pus & sequestra
- surrounded by areas of sclerosis / reactive new bone
3. Soft tissue
- overlying soft tissue is usually indurated, puckered & adherent to bone
- often sinus connecting lesion to skin
Complications
Pathological fracture
- 2° bone destruction & brittleness
Malignant transformation ~ 1%
- sarcoma
- sinus epithelioid ca
Clinical Features
Recurrent flares
- pain & fever
- redness / tenderness
Discharging sinus
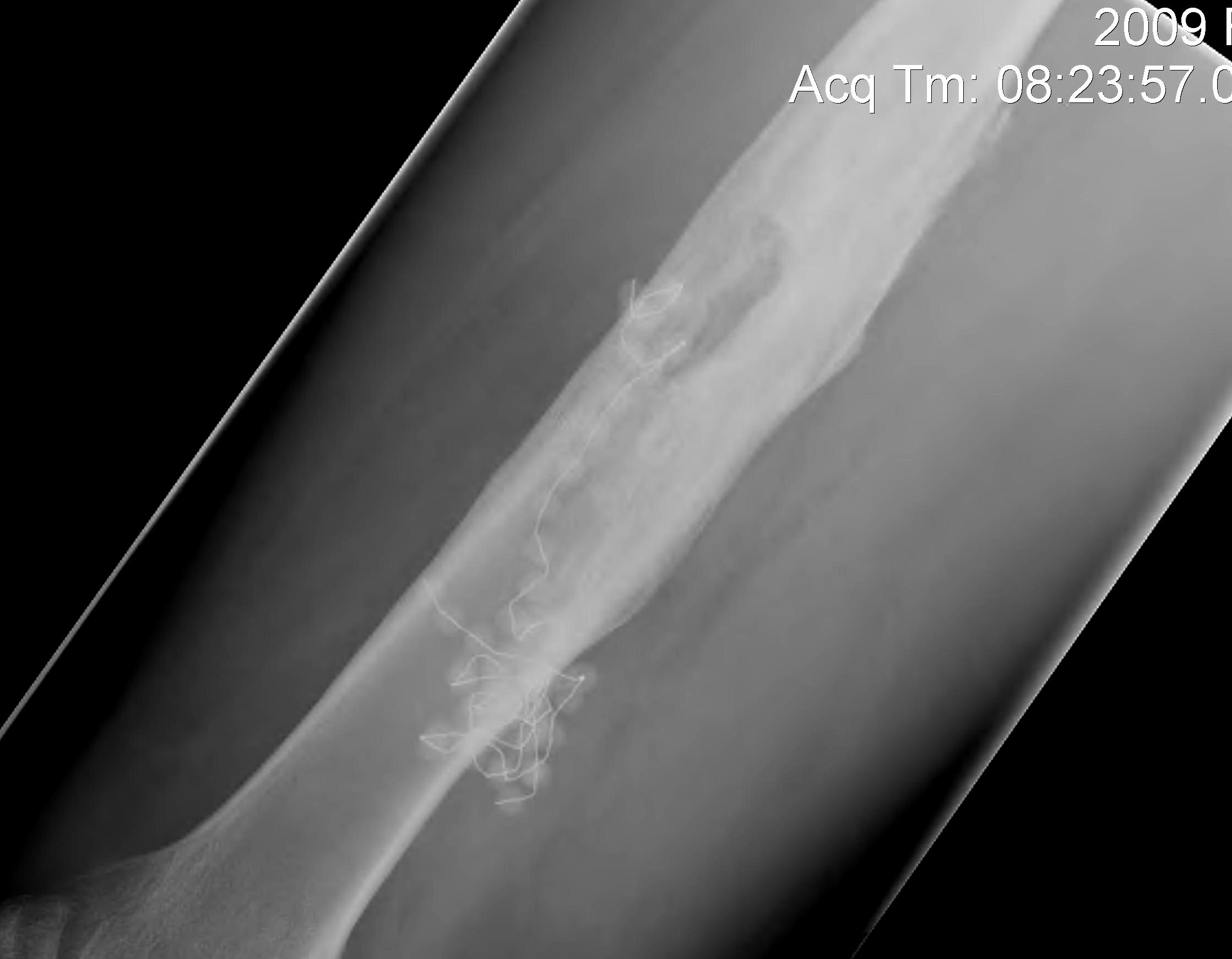
X-ray
Variable amounts of
- patchy lysis with surrounding sclerosis
- ± dense sequestrum
- bone can be deformed

Bone Scan
Increased uptake in lesion
CT scan
Shows bony architecture
Extent of bone destruction
- sequestra
- abscess cavities
MRI
Best to define extent of infection
Bloods
Variable increase ESR & WCC with flares
Repeat MCS / sensitivity changes
Management
Concept Type A / B Host
Classical / Conventional method
- convert infected draining nonunion to non infected, non draining nonunion
- then obtain union
1. Stage host / maximise healing potential
2. Stage infection / MCS / sensitivities
3. Debride all infected bone and ST
4. Stabilise skeleton
5. Eliminate dead space
6. Soft tissue coverage
7. Eradicate infection
8. Deal with bone loss / obtain union
1. Host Factors
Most important in outcome
- control diabetes
- maximise nutrition
- cease smoking
2. Identify organism
M/C/S
Microbiology
- most common S aureus ~ 40 %
- 25 % mixed
- Gram negative 35 %
3. Debridement
Removal of all dead bone
Treat infection like tumour
- meticulous debridement of necrotic tissue
4. Stabilise
Infected non union worst outcome
External fixation / Ilizarov excellent management
- gives stability
- eliminates metal at osteomyelitis site
- obtains union
- deals with bone defect
5. Dead Space
A. Antibiotic beads
- useful in cases unable to immediately graft
- can place flaps over the top & later remove beads
- allows staged bone grafting
B. Papineau open cancellous grafting
Concept
- leave open
- repeated bone grafting, dressings
- "grow bone up" to fill defect
Indications
- defects <4cm
- Type A patients
- stable defect
- subcutaneous bone
Timing of grafting
- depends on appearance of wound 3/52 after initial debridement
- return to OT at 3/52
- if clean --> graft
- if not further debridement
C. Muscle flap
6. Skin Cover
Options
Usually muscle flap with SSG
- crucial to success
- fills dead space
- delivers blood supply / antibiotics / healing
Types
A. Local rotation flap
- gastrocnemius / soleus
- middle or proximal 1/3 tibia
B. Free vascularized flap
- lat dorsi / gracilis
Results
Smith et al J Plast Reconstr Surg 2006
- 10 year audit of 41 patients with chronic osteomyelitis
- 37 had free flap, remainder local muscle flap
- only 2 recurrences (4.4%) which where successfully treated with redebridement
7. Eradicate infection
IV Antibiotics
Repeated debridement
8. Address bony defect
Timing
- usually delay 6/52
- let soft tissues settle, eradicate infection
Options
1. Autogenous cancellous bone graft
2. Autogenous vascularized
3. Structural allograft
- need elimination of infection
- useful in humerus
4. Bone Transport
Indications
- large defect > 4cm
Problems
- high rate of complications
- expertise required
Technique
- debride bone
- acute shortening or delayed docking
- proximal metaphyseal corticotomy
Type C patients
1. Dress sinus / drain acute abscess / suppressive Abx
2. Consider amputation
