Natural history
Low grade parosteal osteosarcoma
- less aggressive locally
- low incidence of metastasis
Epidemiology
Uncommon - 4% of osteosarcoma
Females more common
Natural History
Rajakulasingam et al Skeletal Radiol 2021
- 71 patients
- 43 femur, 14 tibia most common
- 60% low grade, 40% dedifferentiated high grade
- no metastasis seen at presentation on bone scan / CT chest / whole body MRI
- 10% (7 patients) with dedifferentiated tumor had lung metastasis later
- 6/7 had local recurrence
Location
Arises from periosteal surface of bone
Most common in posteromedial distal femur / popliteal fossa
Also tibia & humerus
Clinical
Painless block to knee flexion
X-ray


May look like osteochondroma
- large lobulated broad-based lesion
- mature bone arising from cortex
- underlying cortex may be thickened
- 25% invade periosteum
"String Sign"
- wraps around bone with intervening periosteum
- well-defined radiolucent line between lesion & cortex

CT
Can be used to differentiate from osteochondroma
1. Parosteal OS
- attached to cortex growing into soft tissue
- normal cortex intact

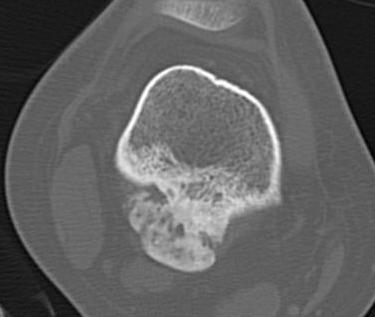
Parosteal osteosarcoma distal femur
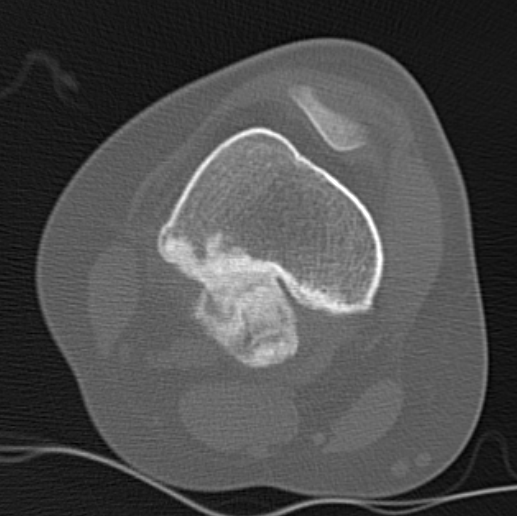

Parosteal Osteosarcoma distal femur
Parosteal Osteosarcoma proximal tibia
2. Osteochondroma
- cortex of bone becomes cortex of osteochondroma
- medullary canal confluent with osteochondroma
- posterior femur rare

Osteochondroma humerus
Differential diagnosis
# Cortical tumors of posterior femur should be considered malignant #
Osteochondroma
Osteoid Osteoma

Osteoid Osteoma anterior tibia
Heterotopic ossification
- not attached to bone

Heterotopic ossification quadriceps following trauma
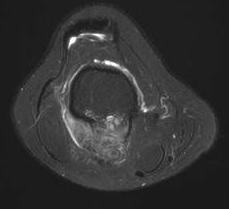
MRI
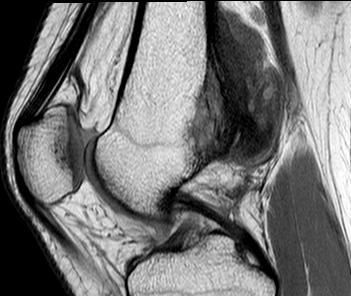
Parosteal osteosarcoma posterior distal femur
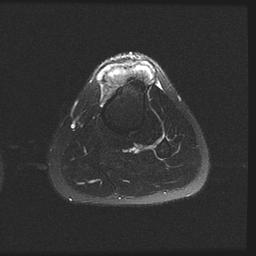
Parosteal osteosarcoma anterior tibia
Parosteal osteosarcoma posterior tibia
Pathology
Gross
Attached to cortex
Does not penetrate medullary cavity
Histology
Low grade
- irregular bony trabeculae and bland-appearing spindle cells within the fibrous stromal tissue
- atypical cells and atypical mitoses are not present
- may have cartilage cap
Can dedifferentiate with much poorer prognosis
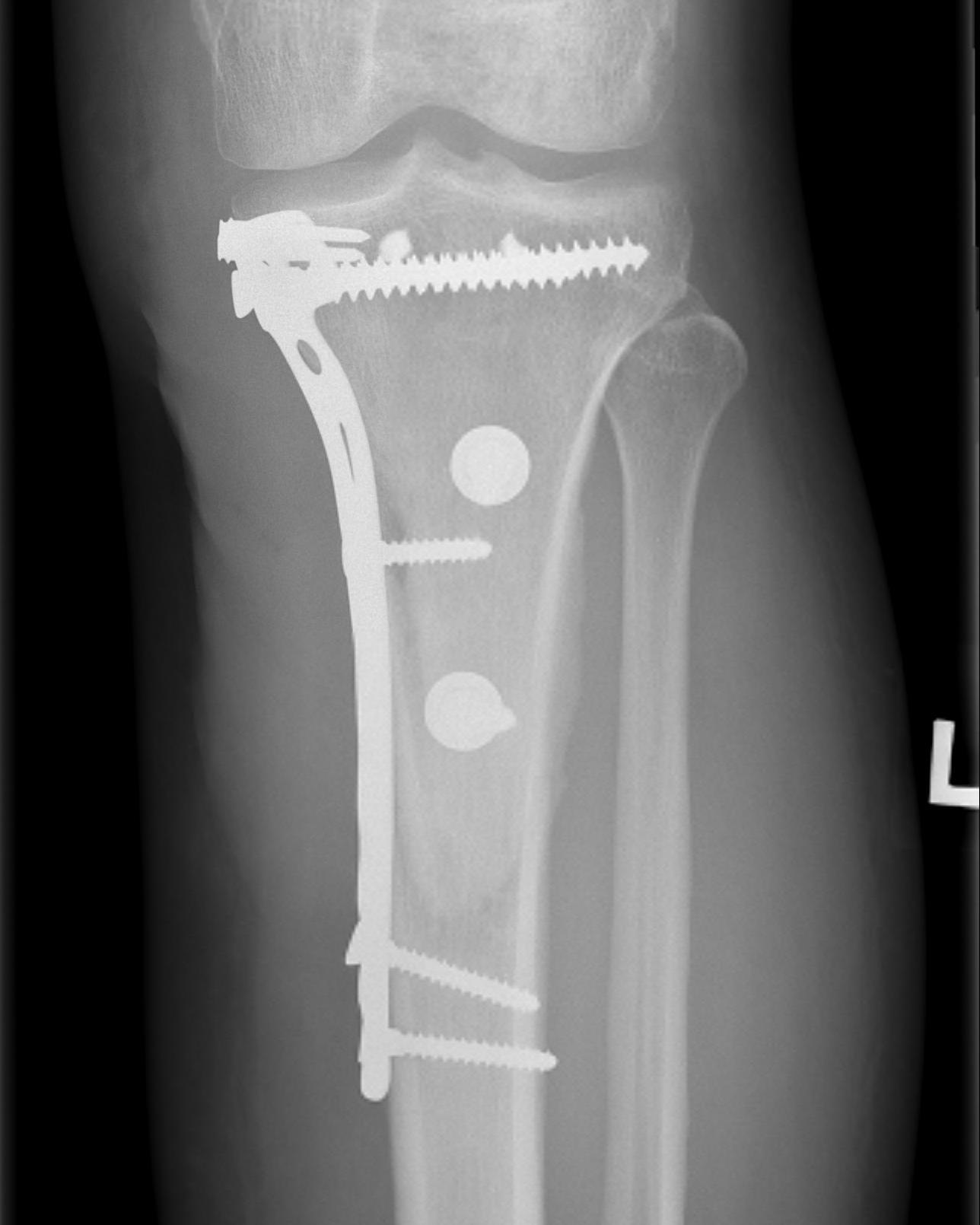
Management
Wide Resection
A. Hemicortical resection and posterior hemicortical allograft reconstruction
- no chemotherapy if low grade




B. Dedifferentiated parosteal Osteosarcoma
Prognosis
Factors
- dedifferentiation
- local recurrence / importance of wide resection
- no obvious advantage with chemotherapy
Survival
- 96% 20 year survival for low grade
Results
Prognosis
Ruengwanichayakun et al Hum Pathol
- 147 low grade parosteal OA
- 5 year survival 96%
- 10 year survival 96%
- dedifferentiated parosteal OS 5 year survival 65%
- 21 patients with 9 year follow up
- 95% survival
- two patients with tumor positive surgical margins on histology
- both had local recurrence, one with recurrence and metastasis
Laitinen et al Bone Joint J 2015
- 80 patients with parosteal osteosarcoma
- local recurrence poor prognosis for survival
- importance of wide surgical margins
Jamshidi et al Orthop Traumatol Surg Res 2022
- 30 patients with low grade parosteal OS
- 14 cases tumor adhered to neurovascular bundle, 16 without
- all patients treated with resection / limb salvage
- 2 local recurrences in each group
Functional outcome
- hemicortical resection and hemicortical allograft reconstruction
- 22 cases (6 parosteal, 6 peripheral chondrosarcoma, 10 adamantinoma)
- all allografts incorporated
- 6/22 (27%) patients had a fracture of the remaining host hemicortex
- good excellent functional outcome in 21/22 patients
- hemicortical resection and hemicortical allograft reconstruction
- 111 cases (18 parosteal, 37 adamantinoma)
- 18% host bone fracture
- 7% nonunion
- 7% infection
- 3% allograft fracture


