
Definition
Facet joint dislocations secondary to flexion distraction injury
Epidemiology
10% of cervical spine injuries
Theodotou et al Neurosurg 2019
- 96 patients
- bilateral facet dislocation in 53%
- spinal cord injury in 81%
- complete spinal cord injury in 32%
- equal distributed C4/5, C5/6, C6/7
Stages
1. Unifacet subluxation - interspinous process widening
2. Unifacet dislocation - 25% anterolisthesis
3. Bifacet dislocation - 50% anterolisthesis
4. Complete vertebral translation - 100% anterolisthesis
Spinal cord injury


American Spinal Injury Association (ASIA) Classification
- A (complete): no motor or sensory
- B (incomplete): no motor, some sensory intact
- C (incomplete): > 50% muscle groups strength < grade 3
- D (incomplete): > 50% muscle groups strength > grade 3
- E (normal) motor and sensory
- 135 patients with facet joint dislocation
- 63% ASIA A or B
- greater severity of neurological injury with bilateral compared with unilateral facet dislocation
- 72% ASIA A or B with bilateral
- 47% ASIA A or B with unilateral
| ASIA | Facet dislocation overall | Unilateral (42) | Bilateral (93) |
| A | 50% | 33% | 59% |
| B | 13% | 14% | 13% |
| C | 13% | 7% | 16% |
| D | 22% | 45% | 12% |
Unilateral Facet Joint Dislocation
Mechanism - flexion / distraction / rotation about contra-lateral intact facet

Unilateral facet joint dislocation on xray - 25% subluxation on lateral X-ray (<50%)





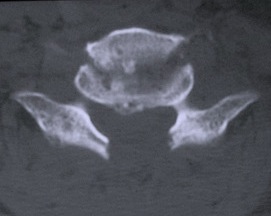
Unilateral facet joint dislocation on CT
Bilateral Facet Joint Dislocation


>50% forward subluxation

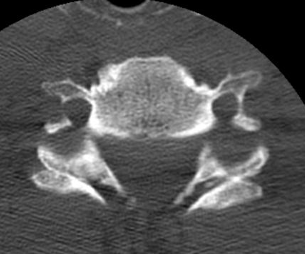
Bilateral jumped facets on CT
MRI
Look for herniated disc
- ? large disc could worsen neurology with skull traction / closed reduction
- ? indication for anterior approach / discetomy / fusion
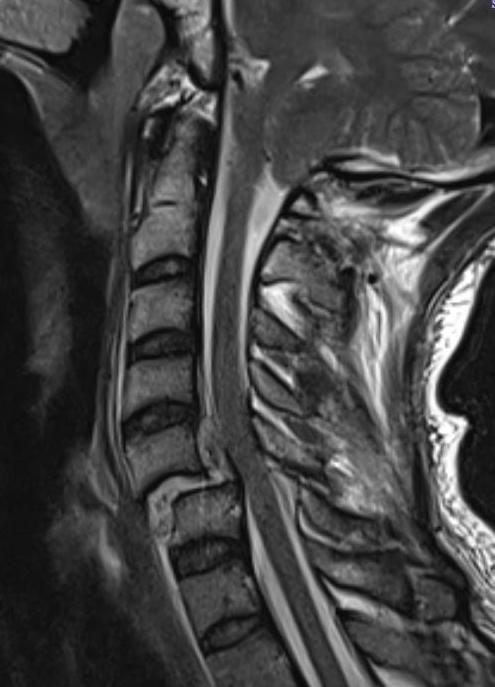
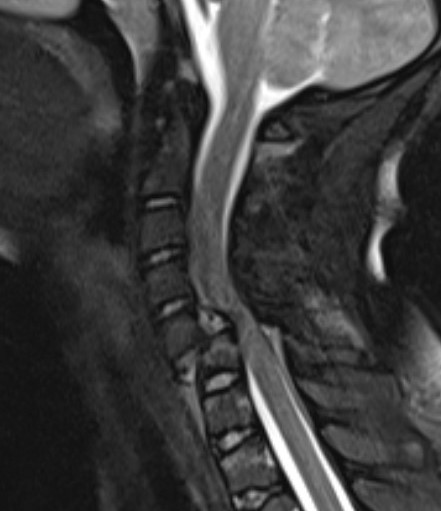
Herniated disc on MRI seen after facet joint dislocation
Management Principles
Issues
Steroids
Timing
Herniated disc
Closed versus open reduction
Anterior versus posterior open reduction
Anterior versus posterior fusion
Spinal cord injury management
Fehlings et al Global Spine J 2017
- evidence of modest improvements in motor function with methylprednisone infusions within 8 hours
Timing
Nagata et al. Eur Spine J 2017
- 30 patients with facet dislocation and complete motor paralysis
- 27% recovered to ASIA C - E
- early reduction (< 6 hours) associated with improved neurological outcomes
- 32 patients with facet joint dislocation and complete paralysis
- 8 reduced within 4 hours - 5 made a complete recovery
- 24 reduced after 4 hours - only 1 made a useful partial recovery
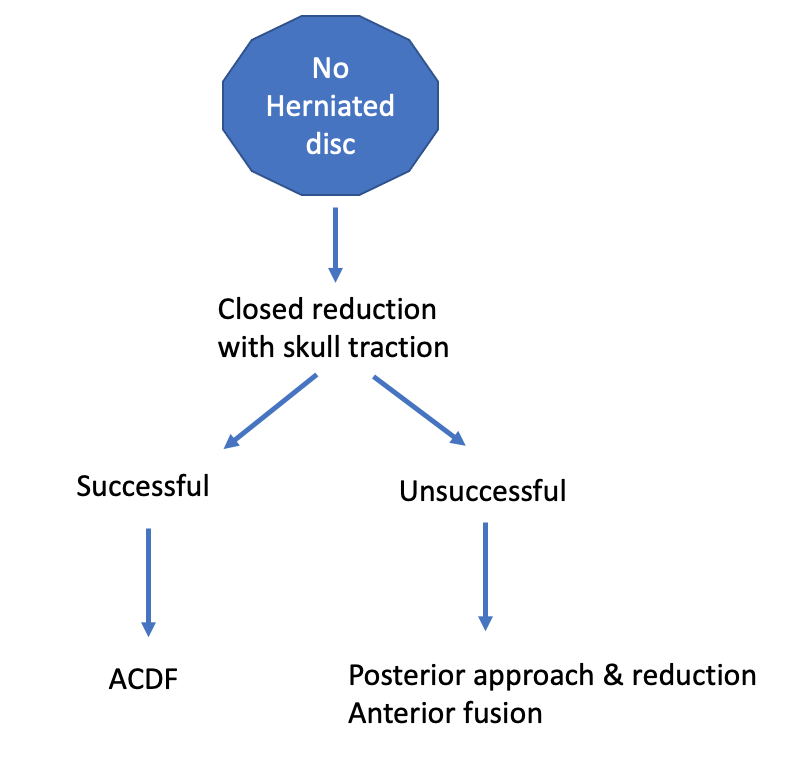
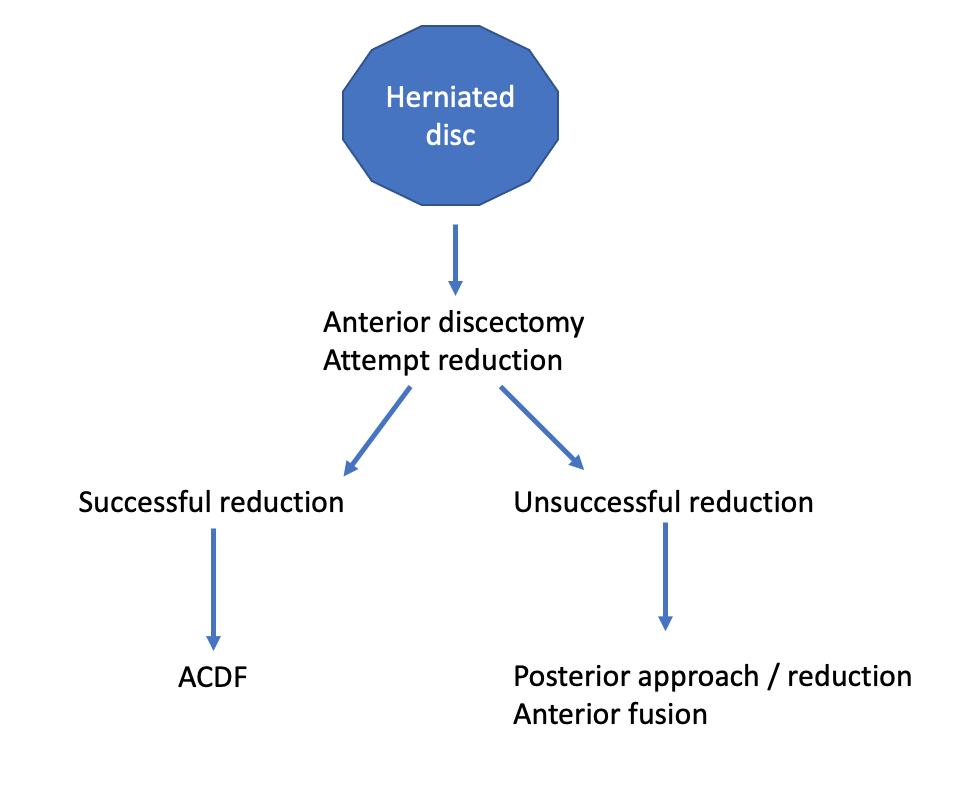
Herniated disc
? need anterior approach and discectomy prior to reduction to avoid spinal cord damage
- systematic review of 197 patients with facet dislocations and herniated disc
- 2 studies with treated with posterior reduction
- 4 studies with patients reduced with skull traction
- worsened neurology seen in one patient
Management plan
Jiang et al Med Sci Monit 2017
- 52 patients with incomplete or normal neurology
Closed reduction
Advantages
In the setting of spinal cord injury, reduced dislocation < 4 hours
Makes surgical fixation and timing easier
Options
Closed reduction
- skull traction
- halo-vest Z-shaped reduction
- manipulation under anesthesia
MUA v skull traction
- 210 patients manipulated under anesthesia vs traction
- traction more successful 88% vs 73%
- traction safer as patient awake & can monitor neurology
Cranio-cervical skull tong traction
Results
Chen et al Zhongguo Jiaoxing 2011
- 68 facet dislocations
- skull traction successful 76% bilateral facet dislocations
- skull traction successful 22% unilateral facet dislocations


Technique
Patient awake and able to communicate if neurology worsening
- best performed in operating room as can use cross table image intensifer
- Gardener Wells tongs 1" above and behind pinna
- below equator / maximum diameter of skull to prevent slippage
- place towels under head to recreate flexion deformity
- start 10 lb for head, then 5 lb for each cervical level every 10 min
- repeat X-ray after each weight increase
- monitor neurological status- if neurology worsens, release all traction
- maximum 40% body weight
- once facet unlocked, removed towels to extend head
Manipulation under anesthesia
Indication
- experienced surgeon
- failure closed reduction
- unilateral facet dislocation
- intention to proceed to open reduction + fusion if required
Technique
- GA + image intensifier + skull tongs
- head flexed 45° & rotated 45° away from side of facet dislocation
- traction in above position, then rotate to side of facet dislocation
- should hear click on reduction
- gently extend to stabilize
- similar method if bilateral, but no rotation (flexion / traction / extension)
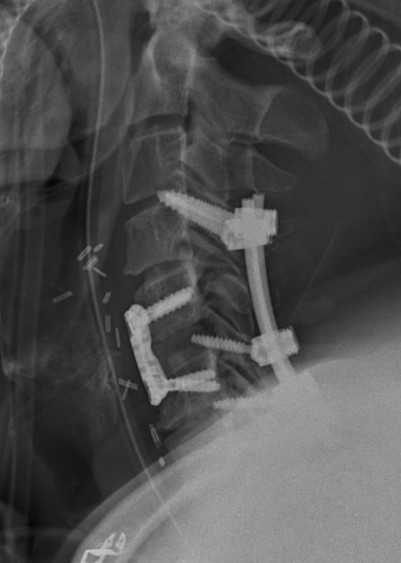
Surgical Fixation
Neurospine 2023 Reduction Techniques PDF
Options
Anterior approach
Posterior approach
Combined 360 degree fixation
Anterior approach and ACDF
Advantage
- lower infection rates
- simpler patient positioning in multi-trauma patient
- can perform discectomy prior to reduction
Disadvantage
- ? more difficult to perform open reduction
- ? stable enough fixation given damage to posterior ligamentous structures
Technique
- decompression / discectomy
- reduction manoeuvre if needed using pins in vertebral bodies
- bone graft and plate

Posterior approach
Advantage
- easier to reduce as direct access to facets
- biomechanically stronger fixation
Disadvantage
- increased wound problems
- ? risk of increased neurology with herniated disc
Technique
- distraction manoeuvre
- instrument between pedicles to reduce
- posterior stabilization or anterior stabilization

Combined anterior and posterior approach
Indication
- severely unstable fractures
- endplate fractures
- facet joint fractures


Results
Operative versus nonoperative treatment
- 90 isolated unilateral facet dislocations
- better outcomes with operative treatment
Dvorak et al Evid Based Spine Care J 2010
- systematic review of 6 papers on unilateral facet dislocation
- treatment failure, persistent pain, and neurological deterioration higher with nonoperative treatment
Anterior alone reduction and fixation
Lee et al. Global Spine Journal 2021
- systematic review of anterior alone reduction and fusion
- 7 studies and 350 patients
- vast majority able to reduce dislocation with open approach
- 1% failure rate with anterior fixation
Theodotou et al Neurosurg 2019
- 96 patients
- 63% had attempted closed reduction, successful in half
- anterior reduction and ACDF
- 92/96 (96%) satisfactory alignment
- 8/96 (8%) required posterior instrumentation for unsatisfactory alignment or loss of position
Posterior alone reduction and fixation
Park et al J Neurosurg Spine 2015
- 21 patients with facet dislocation, 7 with herniated disc
- treated with open reduction and posterior pedicle screw fixation
- patients with herniated disc decompressed via posterolateral approach
Anterior versus posterior
Kwon et al J Neurosurg Spine 2007
- RCT of posterior versus anterior stabilization for unilateral facet joint dislocations
- 42 patients
- anterior approach had lower infection, better union rates, improved xray alignment
- increased risk postoperative swallowing difficulties with anterior approach
Neurological outcome

MRI post reduction and ACDF demonstrating spinal cord injury
- closed or open reduction and fixation
- unilateral facet: 62% improved one or more grade, 24% improved two or more grades
- bilateral facet: 57% improved one ore more grade, 13% improved two or more grades
