Epidemiology
80% cancer patients have spinal metastasis at autopsy
Spine is number one site for bony metastasis (50%)
Cause
Hexagon: PBBLTK
Prostate Breast
Bronchus MM Lymphoma Bowel
Renal Thyroid
NHx
20% of develop cord compression
30% survive >12/12
Pathology
Site
- thoracic spine - 70%
- lumbosacral > cervical spine
Usually multilevel
Vertebral body
- 85%
- usually posterior body near pedicles
- posterior elements uncommon
Symptoms
- neural compression - demyelination / ischaemia
- pathological fracture
- spinal instability
Method of Spread
1. Arterial metastasis
- haematogenous via nutrient arteries
- lung / breast
2. Direct invasion
- through intervertebral foramen
- lymphoma
3. Venous
- via Batson's Plexus
- valveless veins from the pelvis to the internal venous plexus of the spine / prostate
- GIT tumours commonly spread to liver first via the portal system
- then later to bone
4. Lymphatic
Clinical
Pain
- 95% neoplastic pain (night and rest pain)
Weakness
- 75% at diagnosis
- bilateral & symmetrical
Sensory loss
- 50% at diagnosis
- ssually affects the feet first
Loss of sphincter control
- 50% at diagnosis
X-ray
75% have abnormality
Winking Owl Sign / Pedicle loss on AP

Lytic / Sclerotic lesion
- need 30% bone loss to see lytic area
Vertebral body collapse


Bone Scan
Very sensitive
- detect metastasis > 2mm
- screening tool
False positive
- crush fracture
False negative
- myeloma
"Superscan"
- symmetric increased uptake
- metastatic disease
- renal or endocrine abnormality
CT Scan
Define
- bony abnormality
- deformity
- potential instability
Cervical Lesions

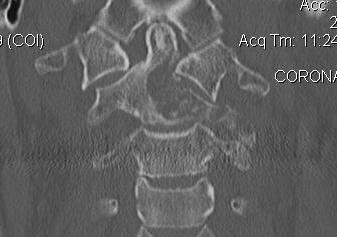
Lumbar


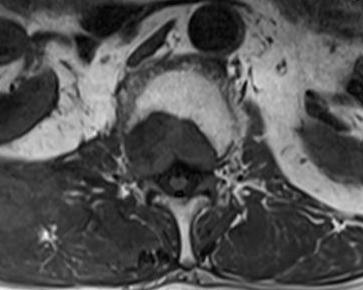
MRI
Define
- soft tissue masses
- nerve and cord impingement



Classification Harrington
Class I
- Minimal bone involvement
Class II
- Bone destruction < 1/2 body / no instability / no cord compression
Class III
- Spinal canal compromise due to epidural disease / no significant bone involvement
Class IV
- Pathological fracture ± deformity / no significant neurological compromise
Class V
- pathological fracture with collapse / instability & neurological compromise
Management
Prognosis
Outcome after treatment = Neurological impairment before treatment
- most ambulatory patients remain ambulatory after treatment
- few paraplegic patients are able to walk after treatment
Radiotherapy v Surgery
Patchell et al Lancet et al
- randomised multicentred trial
- patients with spinal cord compression from metastasis
- trial had to be stopped
- superior results for surgery c.f. radiotherapy and steroids
- improved patient walking ability / retained walking ability
- better maintenance of continence and Frankel grades
Goals
1. Preserve neurological function
- ambulation
- bladder and bowel
2. Pain relief
3. Spinal stability
Decision making
Team approach
- oncologists
- radiation oncologists
- palliative medicine
Issues
- life expectancy
- fitness for surgery
- tumour type
- spinal stability
Harrington Classification
Group 1 & 2 +/- 3
- radiotherapy +/- chemotherapy
Group 4 & 5
- collapse / instability / impending deformity / deformity / neurology
- surgery
Radiotherapy
Sensitivity
Very - myeloma, lymphoma
Moderate - breast, lung, bowel, prostate
Resistant - thyroid, kidney, melanoma
Indications
- Harrington 1 & 2 +/- 3 radiosensitive
- no neurology
- neurology with poor prognosis or unfit for surgery
Operative Management
Indications
- neurology / cord compression
- failure of radiotherapy
- deformity
- instability
- > 3/12 to live
- fit for surgery
Instability
- > 50% height loss
- anterior and posterior columns at same level
- bone loss > 2 vertebrae
Options
1. Decompressive laminectomy
- historical operative associated with poor outcomes
2. Percutaneous PMMA / Vertebroplasty
Indications
- stable lesion

3. Posterior stabilisation
A. Long segment stabilisation


B. Short segment stabilisation + PMMA

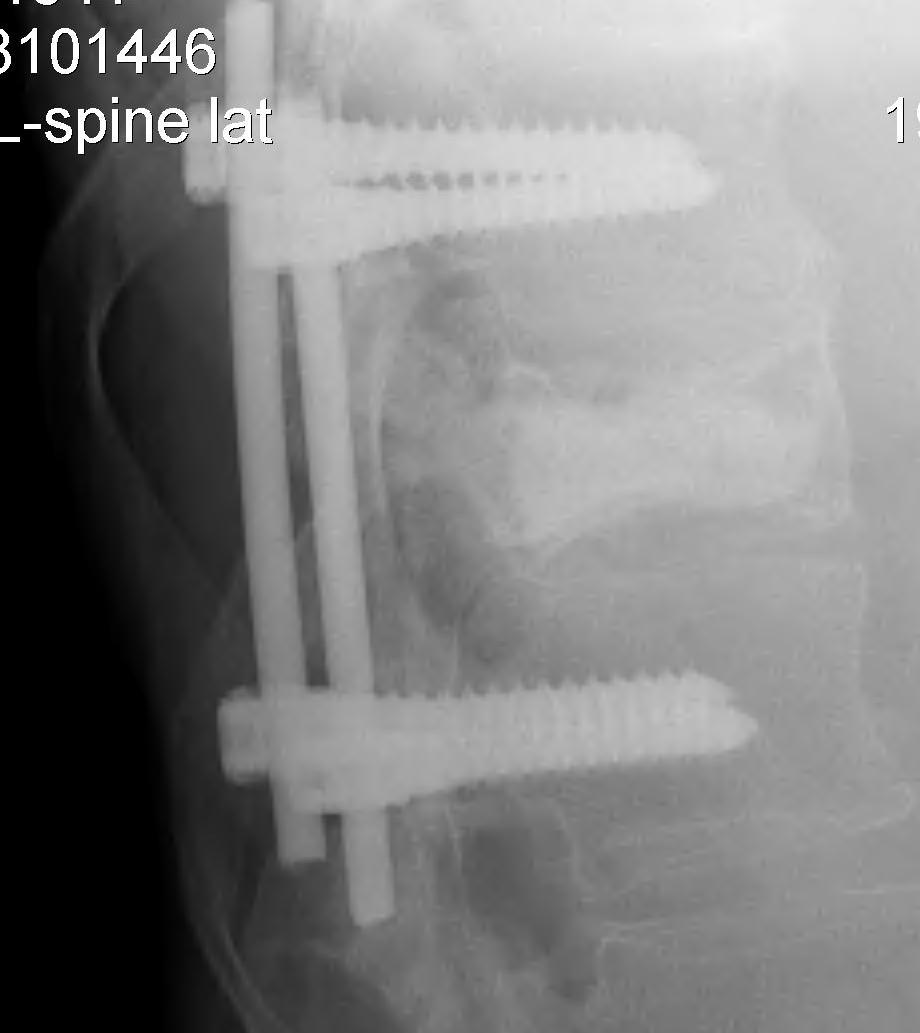
3. Corpectomy / PMMA / Anterior stabilisation
Technique
- remove body and disc to dura
- PMMA sufficient if LE < 6 months
- titanium cage and BG / structural graft if LE > 6/12
- stabilised with anterior plates


Post op Radiotherapy
Week 2 if no bone graft
Week 6 if bone graft used
