Definition
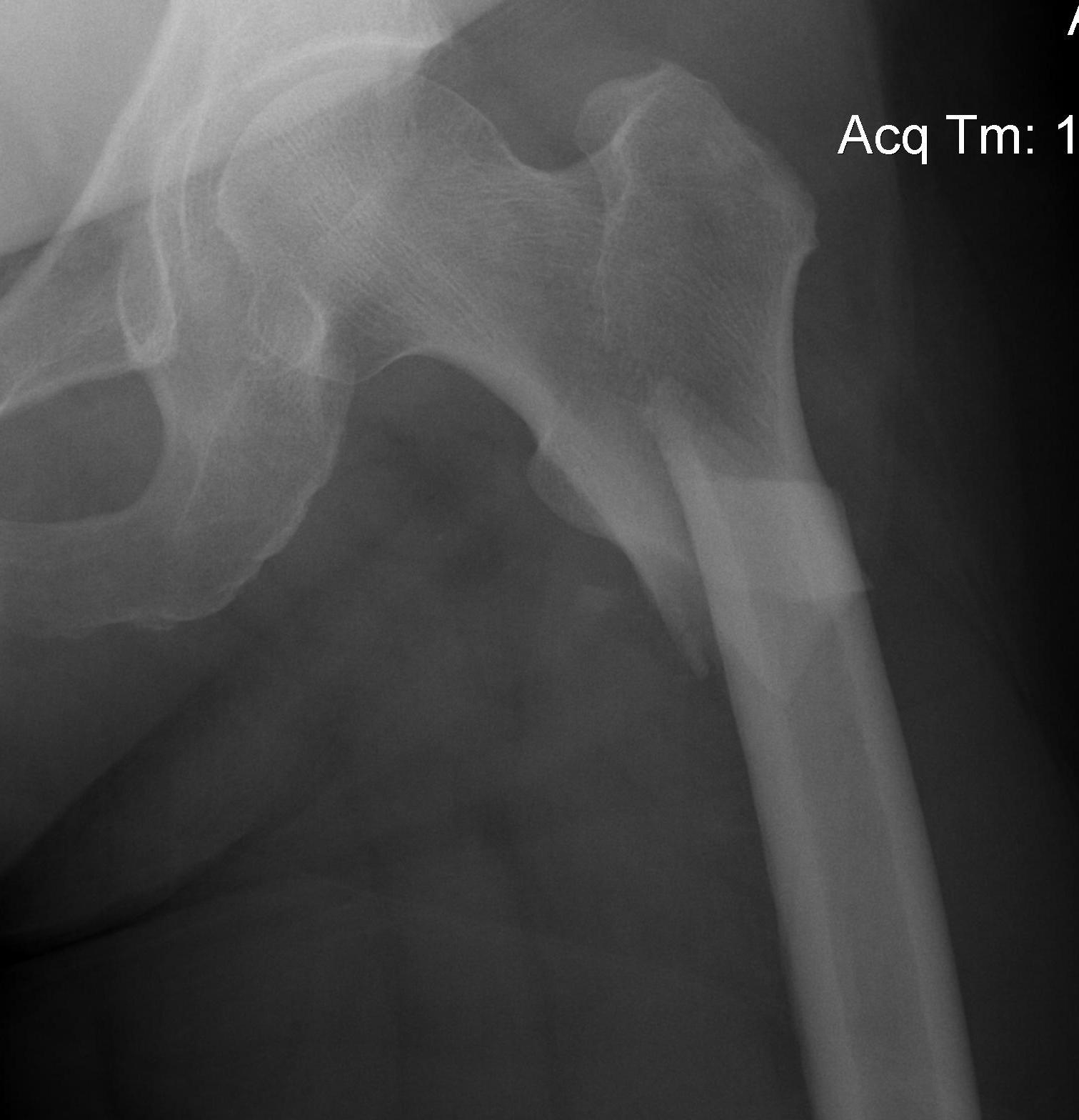
Fracture below lesser trochanter
Proximal 5 cm femoral shaft
Etiology
Young patients / high velocity injuries
Old patients / osteoporosis
AO classification
32-A3: Short transverse

32-B3: Wedge, fragmented

32-C1: Spiral, complex

Russell-Taylor Classification
Typically used to delineate suitability for nail (type I) vs lateral fixed angle device (type II)
Modern locking nails negate this differentiation
Type IA: no extension into piriformis fossa. Simple fracture.
Type IB: IA + comminution
Type IIA: extension through GT into piriformis fossa
Type IIB: IIA + comminution
Fixation techniques
Options
A. Plates
- fixed angle plate / 95o Dynamic Condylar Screw (DCS) plate
- locking plates
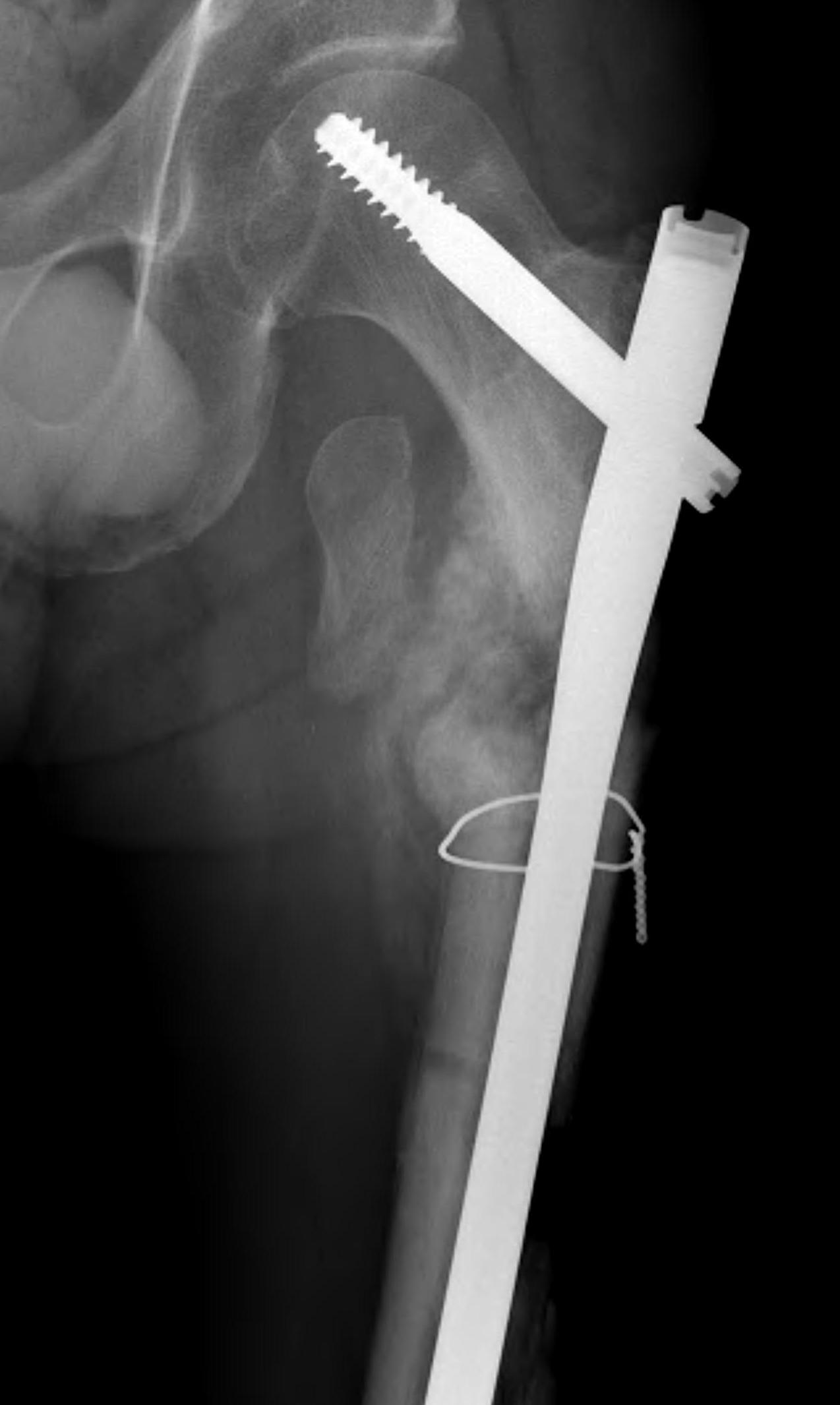
B. Cephalomedullary nails
- gold standard
- load sharing or load bearing, dependant on reduction

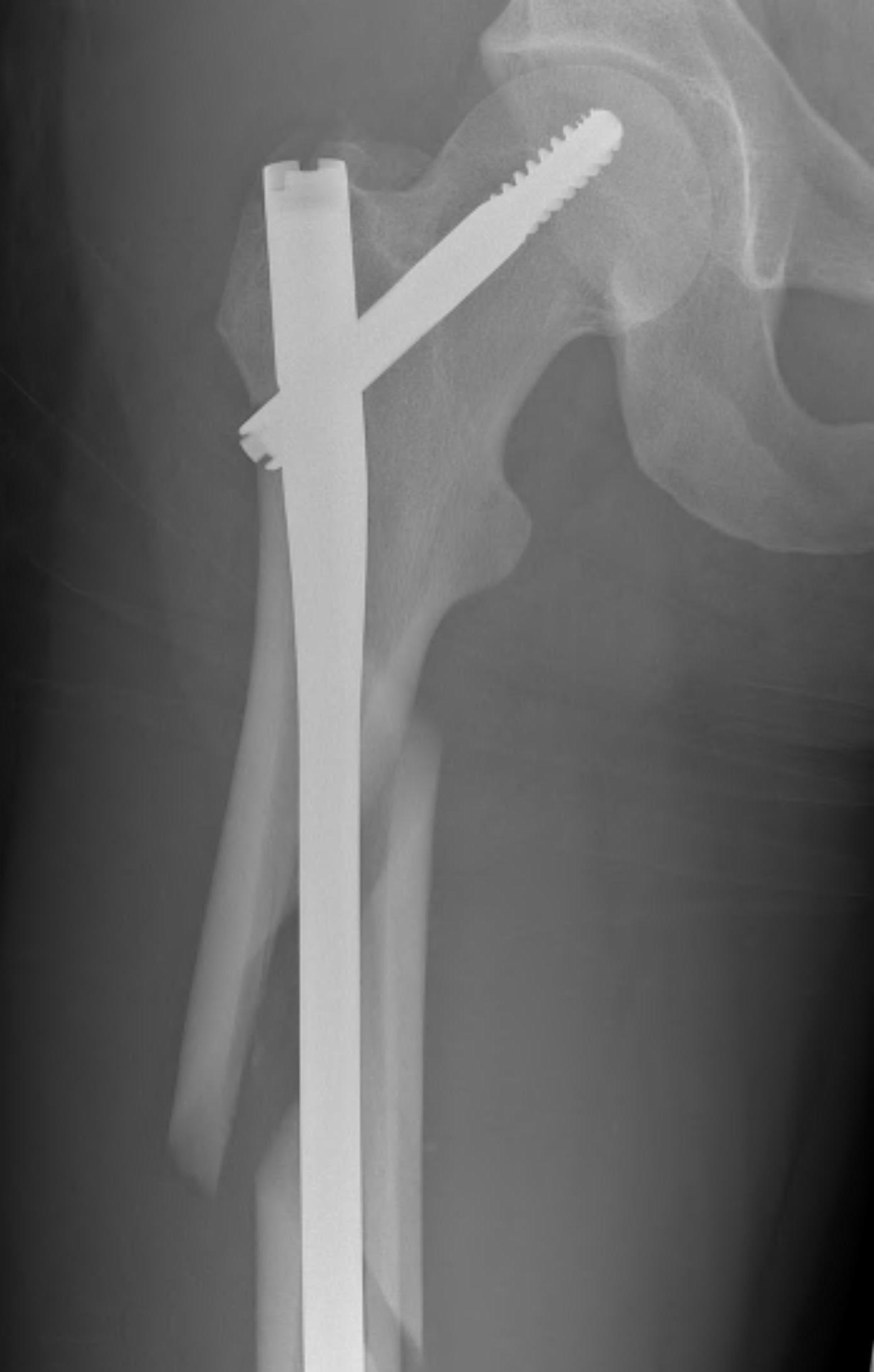

Piriformis reconstruction Gamma nail TFNA with helical screw Intertan nail
Results
Rahme et al J Orthop Surg 2007
- RCT 58 patients
- fixed angle blade plate versus IMN
- revision rate 28% in plate group v 0% in IMN
Collinge et al J Orthop Trauma 2016
- 111 unstable proximal femur fractures treated with proximal locking plate
- 27% underwent second surgery for fixation failure or nonunion
Technique IMN
Vumedi tips and tricks subtrochanteric fractures


Issue
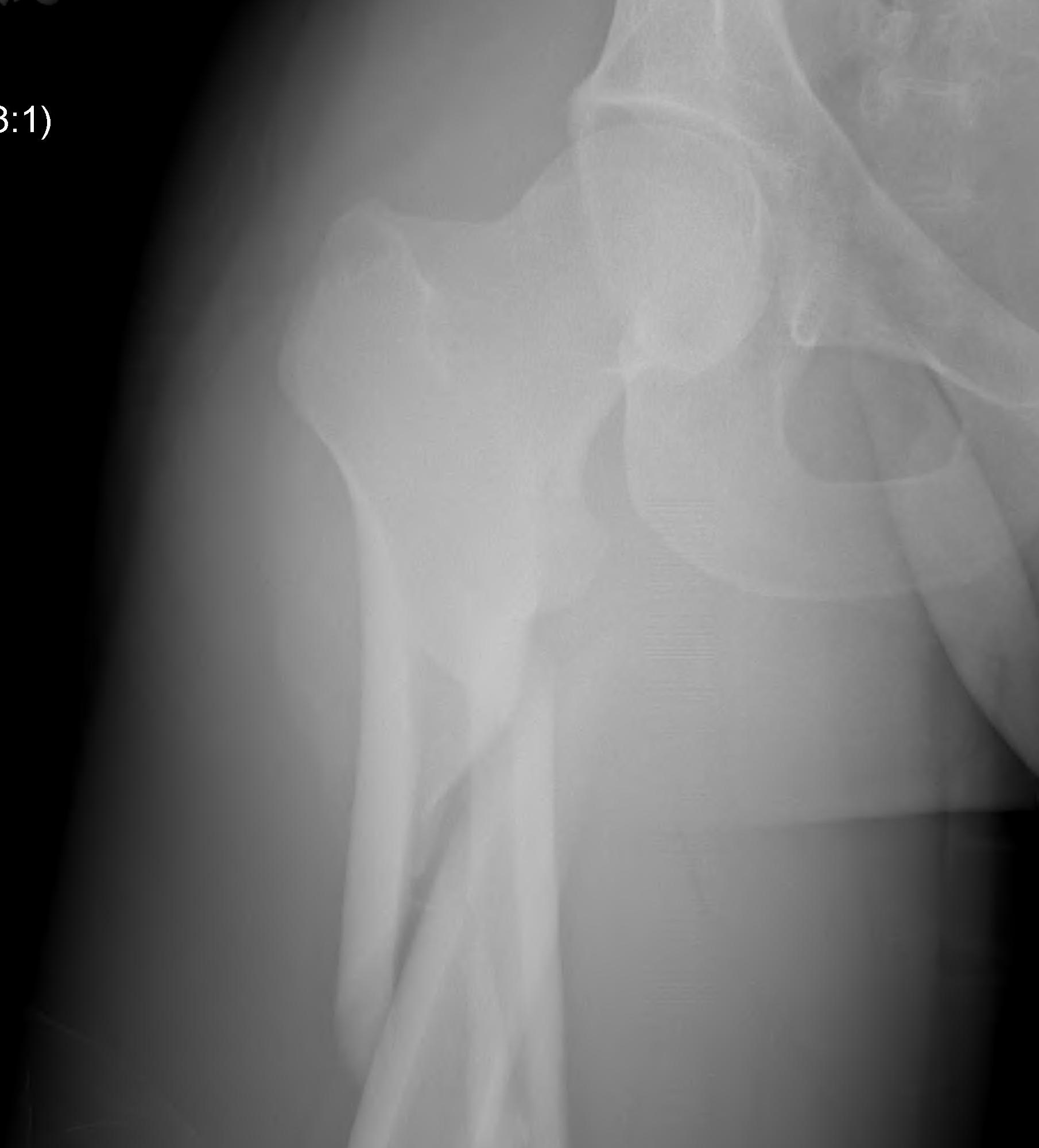
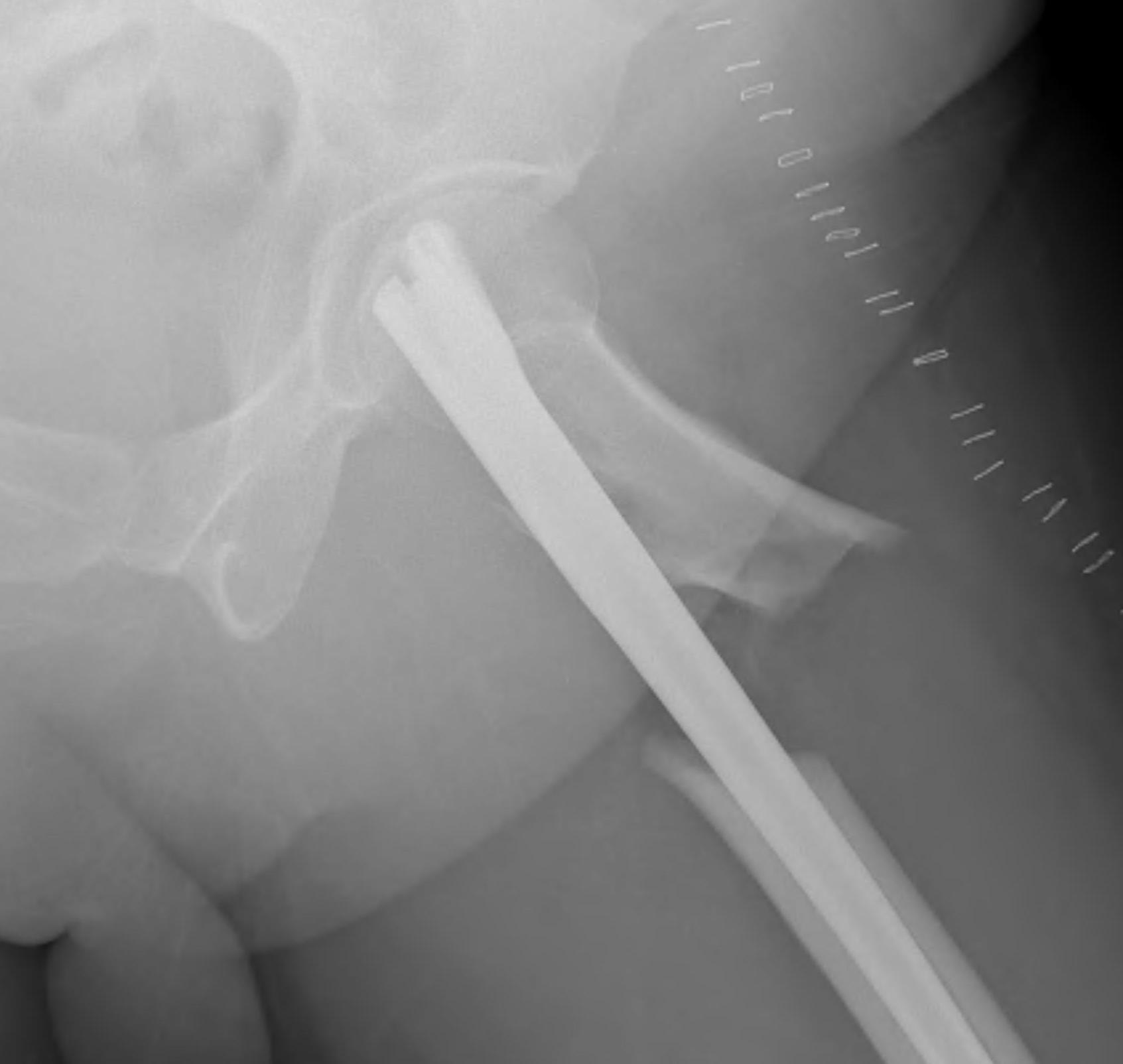
1. Proximal fragment flexed, in varus and externally rotated with distal fragment adducted
- iliopsoas flexes proximal fragment
- abductors cause varus of proximal fragment
- external rotators rotate proximal fragment
- adductors medialize distal fragment
2. Entry point difficult
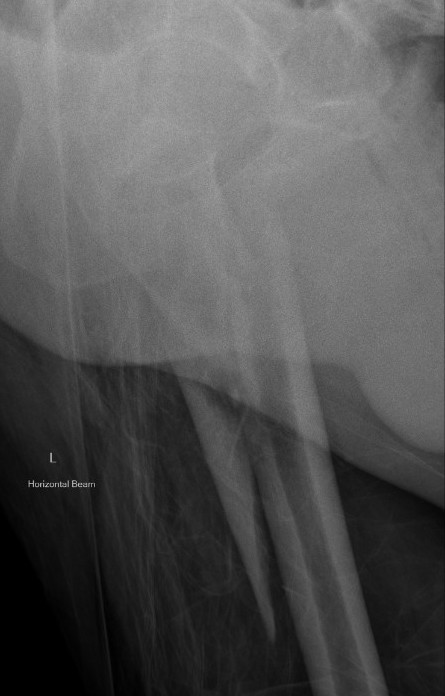
3. Varus malreduction associated with non union
- anatomical reduction key to union
Results
- case series of 102 subtrochanteric fractures treated with IMN
- all nonunion occurred with varus > 10 degrees
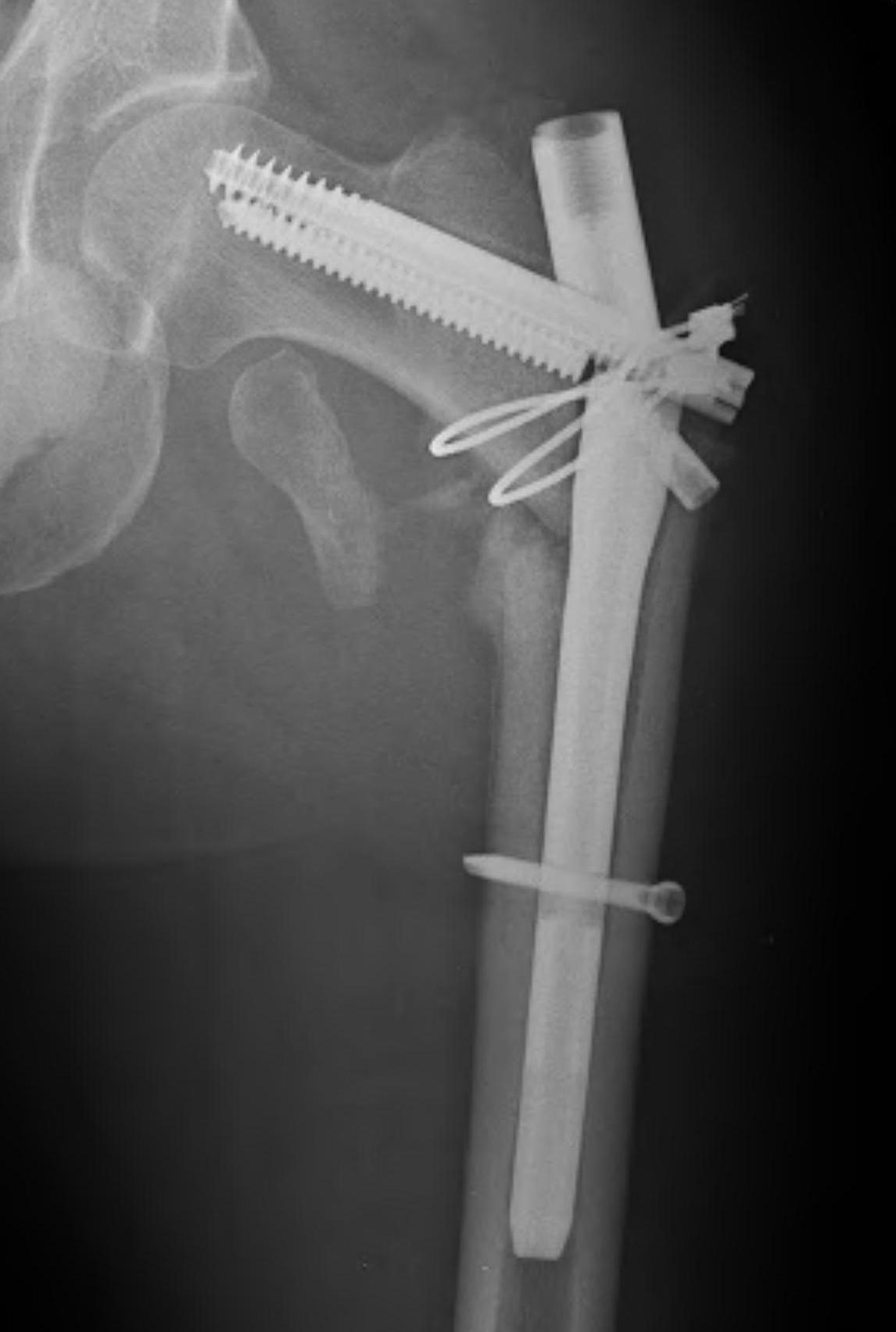
- clamp assisted reduction of displaced subtrochanteric fractures
- all fractures within 5 degrees of anatomical in two planes
- 43/44 fracture united
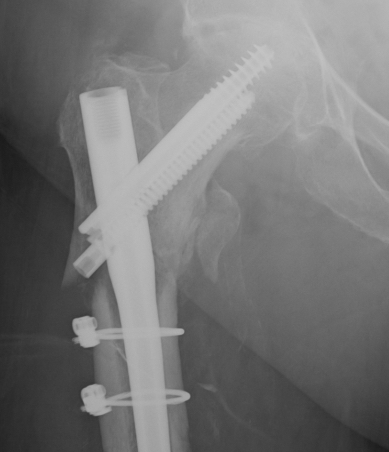
Kim et al Eur J Trauma Emerg Surg 2022
- systematic review of 14 studies and 1700 patients
- faster union and better outcome scores with cerclage wiring
- no difference in non union rates
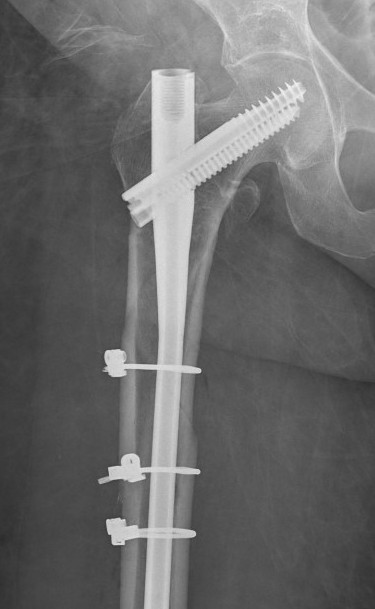
Position
Lateral
- helps reduction of distal fragment to flexed proximal fragment
- easier piriformis access
Supine on traction table
- easier imaging
- longitudinal traction
Entry point
Greater trochanteric
- simple
- need proximal fragment reduced
Piriformis
- may aid reduction, as a trochanteric nail will push proximal fragment into valgus
- more difficult to obtain
Reduction techniques
Yoon et al J Orthop Trauma 2015 Tips and Tricks
Percutaneous
- ball tipped spikes to reduce deformity
- steinman pins to proximal and distal fragment to reduce deformity
- blocking screws laterally and posteriorly in proximal fragment
Open
1. Short transverse fracture
- clamps on proximal and distal fragments and hold reduced
- consider unicortical small plate to hold reduction
- consider blocking screws

2. Longer spiral fractures
- clamping and cerclage wiring with longer spiral fractures

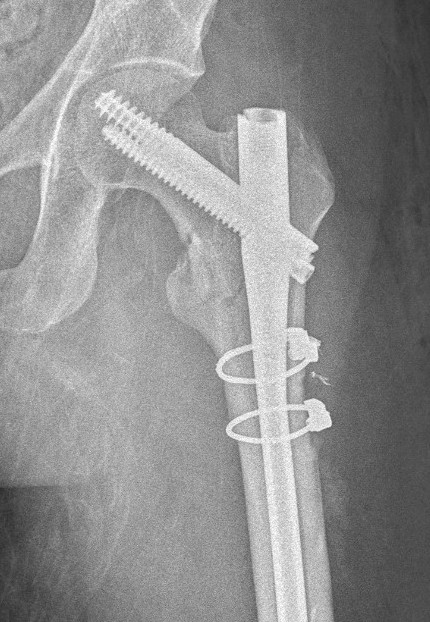



Complications
Varus malreduction



Issue
- trendelenberg gait
- LLD
- non union
Non union

Management Options
A. 95 degree condylar plate
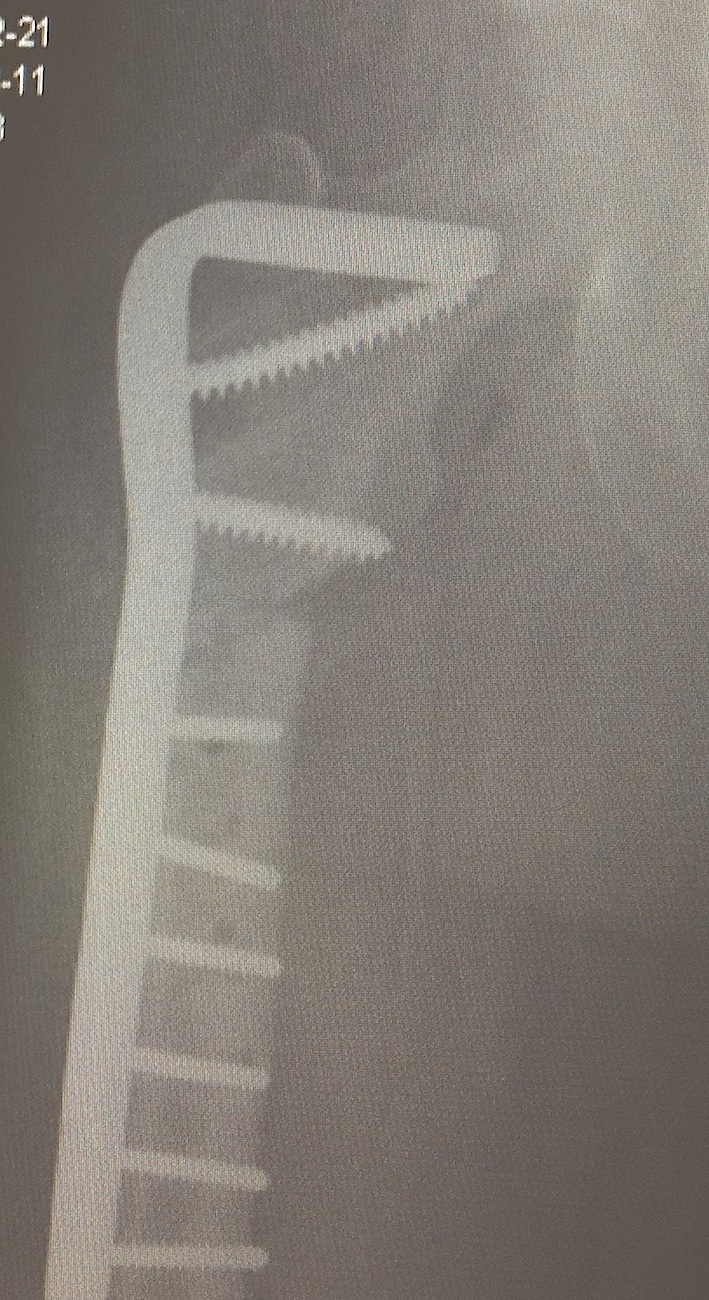
Lotzien et al BMC Musculoskeletal Disorders 2018
- 40 patients with subtrochanteric nonunion treated with DCS
- 37/40 (92%) achieved union
- 13/40 (33%) required additional procedure for union
B. Exchange nailing
C. Hemiarthroplasty / THA



Infected nonunion


