Problems
Instability / Maltracking
Fracture
Loosening or failure of component
Patella Clunk Syndrome
Extensor Mechanism Rupture
Incidence
PFJ complications 5%
PFJ Instability / Maltracking
Effect
Catastrophic wear
Component loosening
Pain
Fracture
Aetiology
1. Component Malposition / Malalignment
A. Internal rotation of the femoral or tibial component
- increases the Q angle

B. Medialisation of femoral component
C. Axial Malalignment
- valgus > 10o
D. Lateralisation of patella button
E. Overstuffing of the patella femoral joint
- tightens the lateral retinaculum
2. Poor patellofemoral Component design
A. Poorly designed trochlea / patella
B. Hinged or constrained knee
- normally get IR with early flexion
- this medialises tibial tuberosity
- constrained TKR don't do this and have a lateral vector
3. Soft tissue balancing
Tightness of lateral retinaculum in long standing valgus
- at end of OT should track centrally without any external pressure
- no tilt
- otherwise lateral release +/- patella resurfacing

Investigation
Examination
- Assess tracking
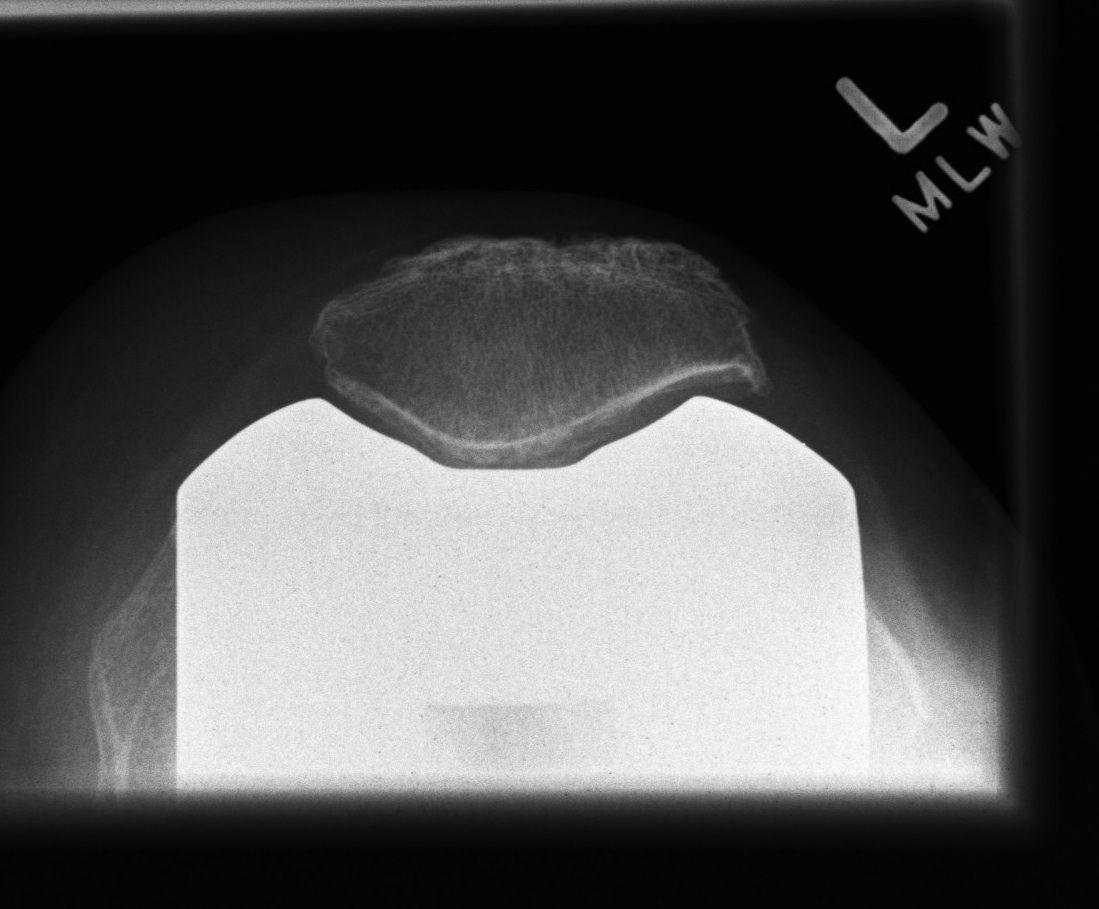
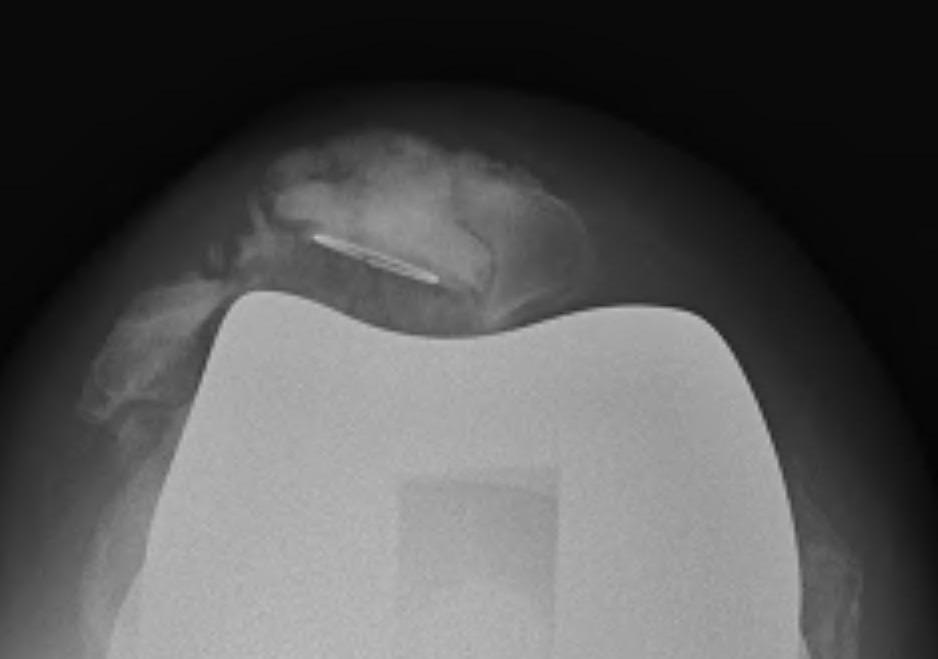
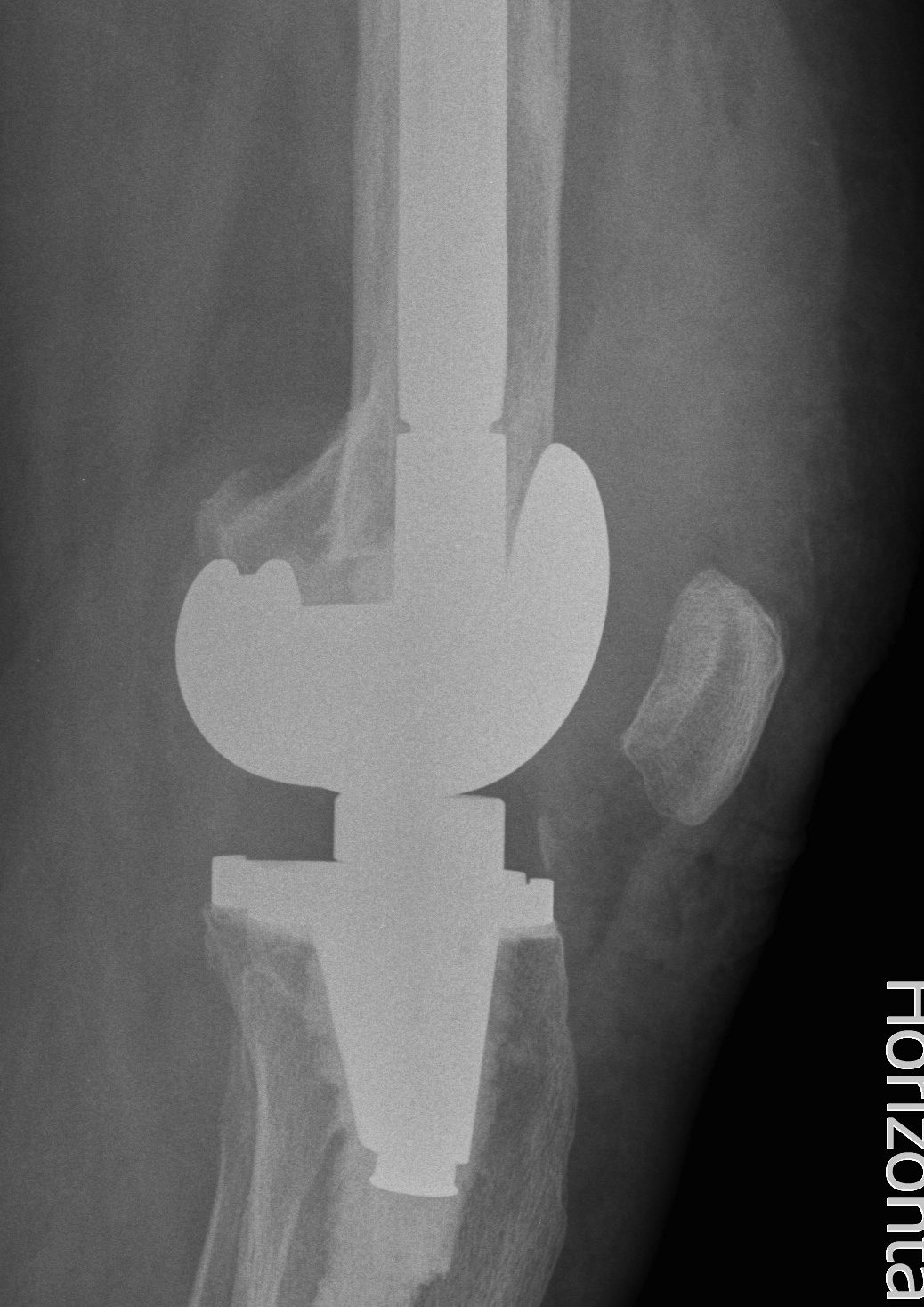
Xray
- skyline views
- lateral tilt / subluxation
![]()
![]()
CT
- rotational profile of the components
Management
Non-Operative
- VMO exercises
- often unsuccessful
Acute trauma
- patella has been tracking centrally since OT
- not since acute trauma
- immediate capsular repair is indicated
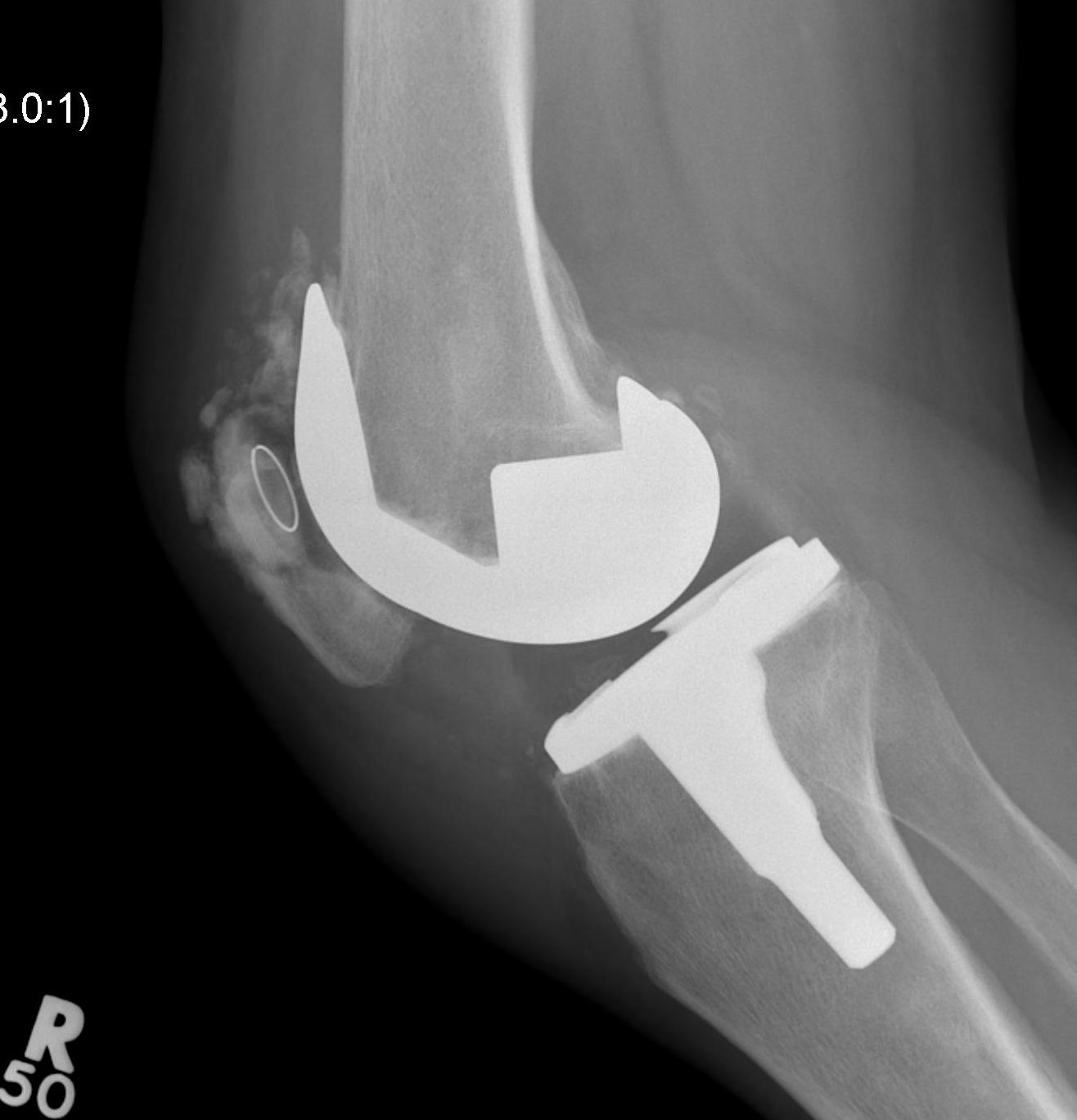
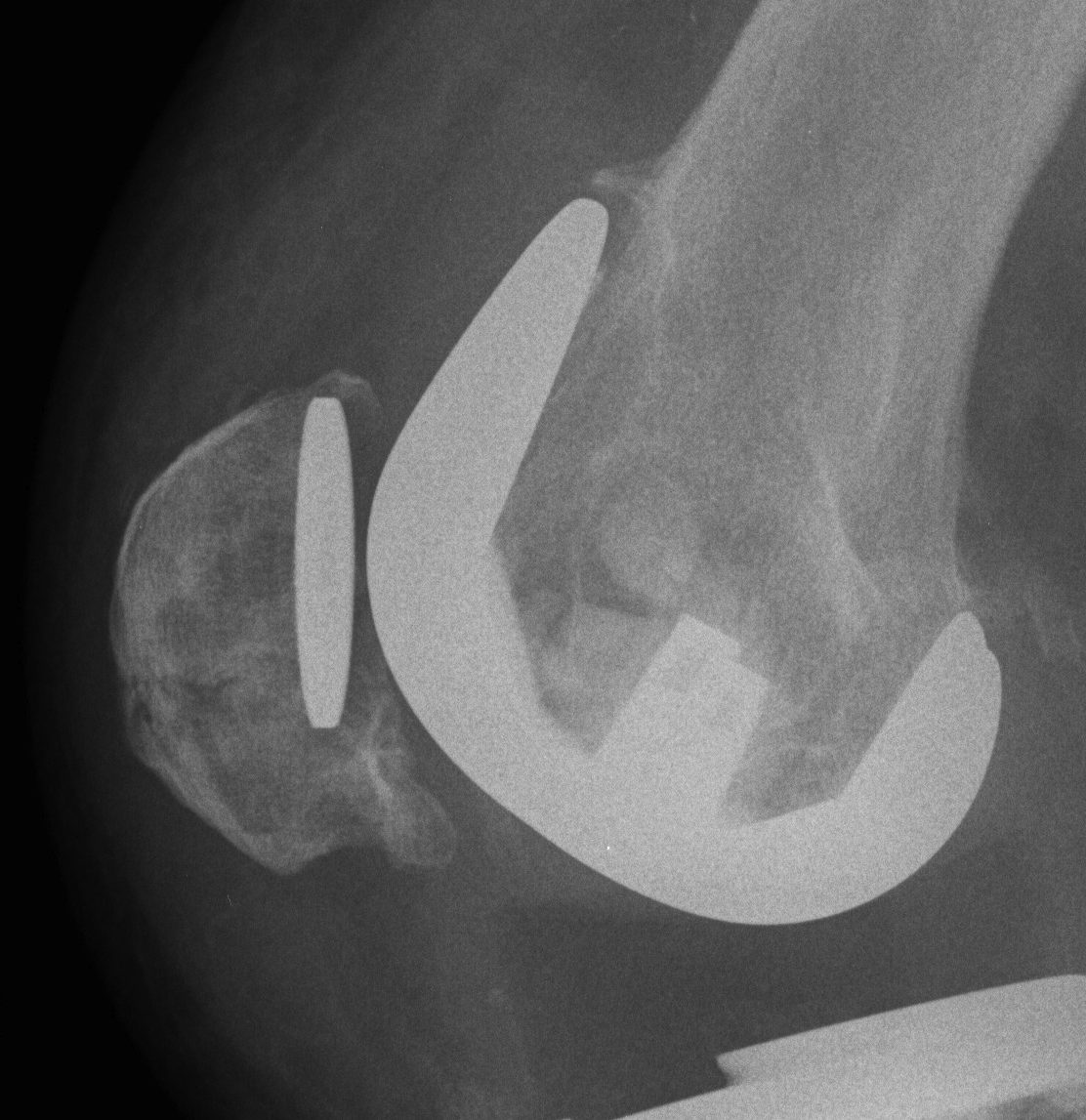
Surgical options
1. Lateral release + Patella resurfacing
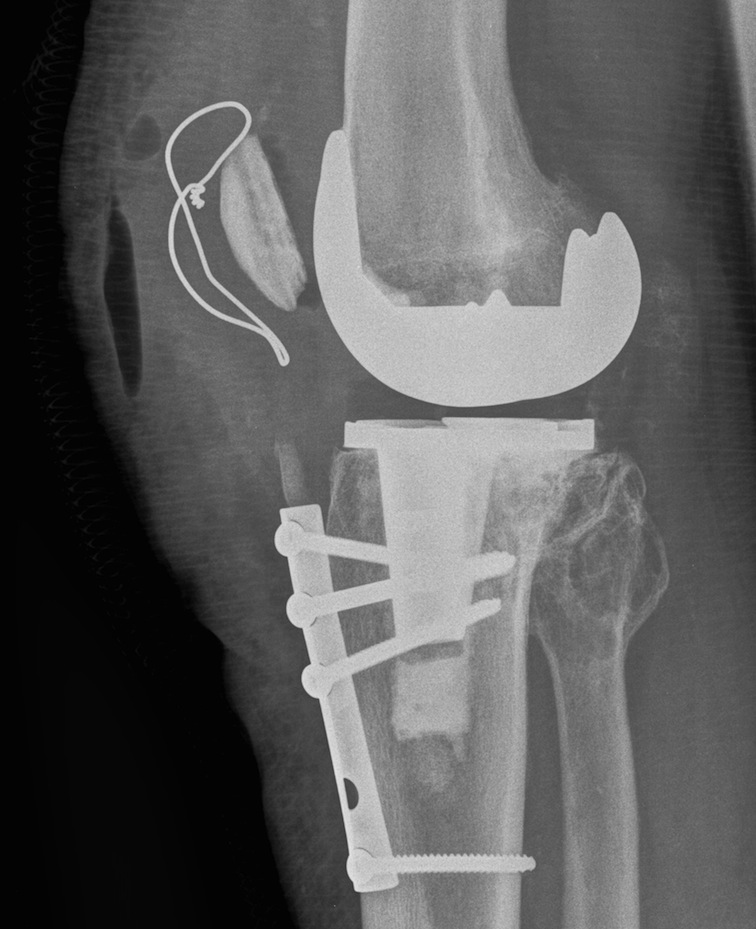
2. Tibial tuberosity transfer +/- MPFL reconstruction
![]()
![]()
Barber et al Arthroscopy 2008
- 91% successul in eliminating instability in 35 knees
- used Elmslie Trillat
3. Revision
Options
- medialise patella component
- revise malrotated components
Patella Fracture

Incidence
Uncommon
- 0.1% Primary
- 0.6% Revision
Causes
1. AVN
Disruption of patella blood supply
- patella turndown
- medial approach and lateral release
2. Excessive / asymmetric patella resection
- at least 15 mm native patella must remain
3. Large central hole
- increases strain more than small peripheral holes
4. Anterior patella perforation
- more common with inlay
5. Increased PF strain
- oversized or anterior femoral component
- oversized patella component
- patella baja
Management
Non-Operative
Indications
- extensor mechanism intact
- patella component stable
Treatment
- immobilse for 6 weeks then progressive ROM
Operative
Indications
- loose component or ruptured extensor mechanism
Treatment
A. Patella ORIF if component stable
B. Removal component if unstable + Patella ORIF
Patella Component Loosening
Incidence
Cemented patella
- < 2%
Uncemented higher
- 0.6% - 11.1%
Associations
Metal backed designs
Uncemented
Fracture / AVN of patella
Excessive bone removal
Management
A. Remove and leave
B. Revision
- need > 10 mm bone left
C. Patellectomy
Patella Clunk Syndrome
Symptom
Clunk with knee extension
- as patella exits groove at 30-45° extension
Complain of symptoms when rising from chair or climbing stairs
Pathology
Fibrous nodule at junction of posterioraspect of patella and quadricep tendon
- with flexion enters trochlear groove and gets trapped as go back into extension
- usually due to entrapment at superior flange of femur
- inflammation and a synovial proliferation
Causes
Increased incidence in PS knees
Newer designs
- deeper patella groove
- more posterior femoral box
Investigation
Can visualise nodule on ultrasound
Management
Arthroscopic debridement
Dajani et al J Arthroplasty 2010
- good result in 15 knees
Rupture of Extensor Mechanism
Incidence
0.17-2.5%
Causes
Usually post operative, insidious and due to a vascular insult
Lateral release - devascularises tendon
Closed MUA of knee
Osteotomy of tibial tuberosity
Revision TKR
Prevention with surgical technique is imperative
Effect
Debilitating extensor lag
- can be about 50o
- operation improves this to about 20o
Can predispose to knee dislocation / post jump
Operative Management
1. Primary repair with autograft / allograft reinforcement
- staples, wire reinforcement
- hamstring reconstruction (leave attached distally)
- achilles tendon allograft
- Lars ligament reinforcement
Usually left with extensor lag

2. Chronic rupture / failed repair
Must deal with patella baja
- combine repair with proximalization of tibial tuberosity

3. Revise to constrained prosthesis if required
- PS component
- loss of mechanical advantage of quads
- extensor lag
- anterior translation of femur on tibia once the PCL stretches
