Incidence
Most common lower limb neuropathy
Aetiology
Valgus TKR - 3%
HTO - 10%
Direct Trauma / Compression
Knee Dislocation
Tibial fracture
Cast / Dressing
Lateral Meniscus Repair
Anatomy
Bound to periosteum of fibula in proximal 40mm
- safe between 40-70 mm
- high risk 70 - 160
Perform osteotomy between 40-70mm from head or >160mm
CPN
- L4,5 S1,2
- runs along biceps femoris (supplies short head)
- over lateral head gastrocnemius
- penetrates posterior intermuscular septum
- adherent to periosteum of fibular neck
- divides into superficial and deep peroneal nerves
SPN
- passes between PL and PB (supplies them)
- runs along lateral cortex of fibula
- runs between EDL and PLB
- pierces fascia 10-12 cm above lateral malleolus
- at some points is only 5mm from anterolateral fibula
- 6 cm above distal fibula, divides into intermediate and medial dorsal cutaneous nerves
DPN
- courses anteriorly around fibula neck
- runs along anterior cortex of fibular for 3-4 cm
- passes under intermuscular septum between lateral and anterior compartments
- enters the anterior compartment
- quite tethered here so is more at risk that SPN
- supplies muscles of the anterior compartment
- Tibialis anterior is first branch off DPN
- runs with anterior tibial artery between EHL and EDL (Tom Had A Night Down Town)
- passes under the extensor retinaculum
- branch to EDB, sensation to first web space
Clinical
Injury to CPN & DPN both cause foot drop
Injury to CPN
- foot drop & supination deformity during swing phase
- loss of T nnt (DF)
- loss of peroneus longus / brevis (evertor)
Injury to Deep Peroneal
- only foot drop
- peronei supplied by SPN
Injury in THR
- sciatic nerve has tibial & peroneal components
- in sciatic nerve palsy usually lose one or the other
- tibial nerve supplies all hamstrings except short head biceps
At hip only 20% of volume of sciatic nerve is nerve fibres
- remainder is adipose tissue
- repair here often fails as unable to oppose nerve fibres
DDx
DDx CPN at fibula head vs Peroneal component of sciatic nerve at hip
- EMG of short head of biceps
- denervation means sciatic nerve
DDx CPN v L5 nerve root
- abductor function lost with L5 nerve root injury
NHx
Some authors report resolution of palsy if left long enough
Dee
- 30% recover
- 10% partial recovery
- 60% no recovery
Rose, Ranawat and Insall 1982
- 6/23 cases who had motor loss recovered completely
Asp and Rand
- 26 palsies 8998 TKR
- complete motor and sensory only 7/19 full recovery
Management
Non operative Management
Valgus TKR with immediate post-op palsy
Remove all constricting dressings
- flex to 30-40°
- ensure no compartment syndrome
- evacuate haematoma if present
Operative Management
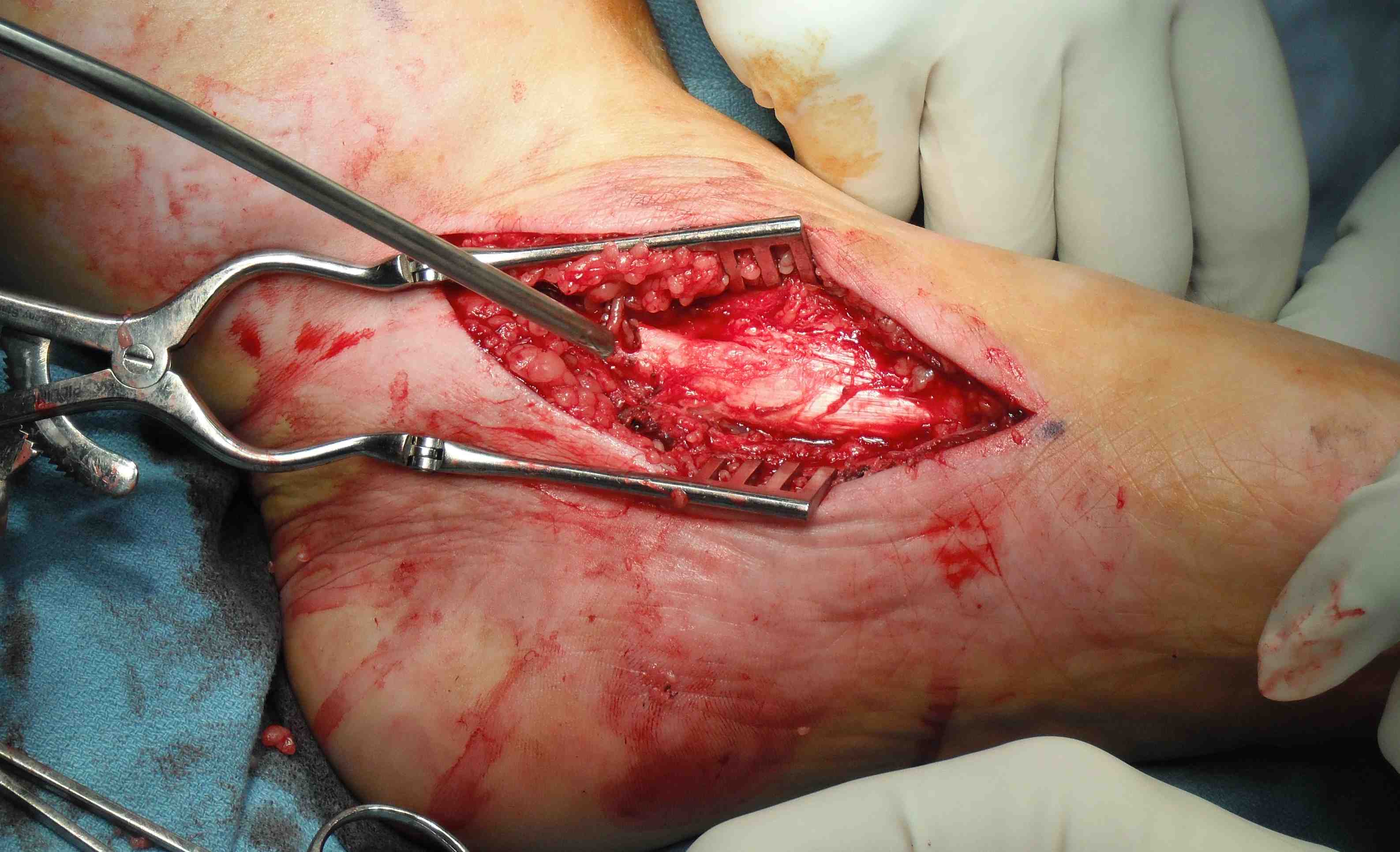
1. Neurolysis
A. Krackow 1996
- patients with CPN palsy post TKR
- EMG and NCS at 3/52 / repeat at 3/12
Operative exploration at 4/12 if persistent dysfunction
- release of nerve
- findings at surgery
- epineural fibrosis
- bands of fibrous tissue constricting nerve at fibula head / proximal origin peroneus longus
- felt CPN palsy was not unlike peripheral compressions elsewhere & therefore treat as CTS
- 31 patients minimum 2 months post-op
- 97% improved post decompression
Full recovery of motor function regards time from injury
- < 6/12 8/8
- 6 - 12/12 4/5
- 1-2 year 7/11
- > 2 years 6/7
Non operative
- only 3 of 9 treated non-op reported improvement
B. Kim et al Neurosurg 2004
- neurolysis if recordable action potential
- 107/121 (88%) recovered useful function
2. Nerve repair
Kim et al Neurosurg 2004
- 318 injuries
- 19 patients with end to end
- 16/19 good results at 2 years
3. Nerve grafting
Siedel et al Neurosurg 2008
- 70% good results in patients with nerve in continuity (nerve stimulator)
- had external or internal neurolysis
- only 28% good functional result from sural nerve grafting
- related to graft length
- good result in 44% if graft < 6 cm (4/9)
- good result in 11% if graft > 6 cm (1/9)
4. Tendon transfers
Tibialis posterior transfer
- passed through interosseous membrane
- sutured to T ant, EHL, EDL

Results
Ozkan et al J Reconstr Microsurg 2009
- 34/35 achieved DF to or above neutral
Diagnostic Dilemmas
1. No anterior / lateral / posterior compartment working
DDx
A. Compartment syndrome
- all 4 compartments
- huge compartment syndrome
B. Sciatic Nerve
- no hamstrings
C. Spine
- taken out L4,5 & S1
- massive disc on MRI
2. No anterior / lateral
DDx
A. CPN knee
- normal short head biceps EMG
B. CPN higher
- abnormal short head biceps EMG
3. No posterior compartment
DDx
A. Compartment syndrome
- deep and superficial posterior
B. Tibial Nerve
- no hamstring function
C. Spine
- S1 compression
- peroneals should be gone as well
4. No Posterior / Lateral
DDx
A. Spine
- S1 compression
B. Compartment syndrome
5. No Anterior
DDx
A. Compartment syndrome
B. Deep peroneal injury
