Ossification
Patella may develop from one or multiple ossification centres at 3 years
Failure of centres to fuse may produce bipartite or tripartite patella
- usually bilateral and painless
Classically superolateral
Classification Saupe
I Inferior Pole 5%
II Lateral 20%
III Superolateral 75%
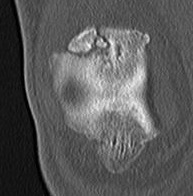
Xray


CT
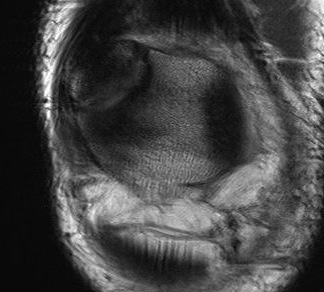
MRI
Look for increased uptake ? symptomatic
Clinical
1. Overuse
- pain may result from repetitive microtrauma
- injury to synchondrosis
- point tender & swollen
2. Acute injury
- can get acute injury with minor separation
- reports of bipartite patella healing post injury
- check SLR to ensure quadriceps tendon intact
Management
Non operative Management
Majority will settle with non operative management
- mmobilisation for 4 weeks
- avoid impact sports
Ultrasound / Exogen
- reports of healing bipartite patella post injury
Operative Management
Options
Lateral release
Adachi et al Arthroscopy 2002
- lateral release performed
- excellent results in 13 and good in 4
- nearly 2/3 healed and remainder partially healed
- bone union more likely in patients < 15
Mori et al Am J Sports Med 1995
- 15/16 united at 8 months post lateral release
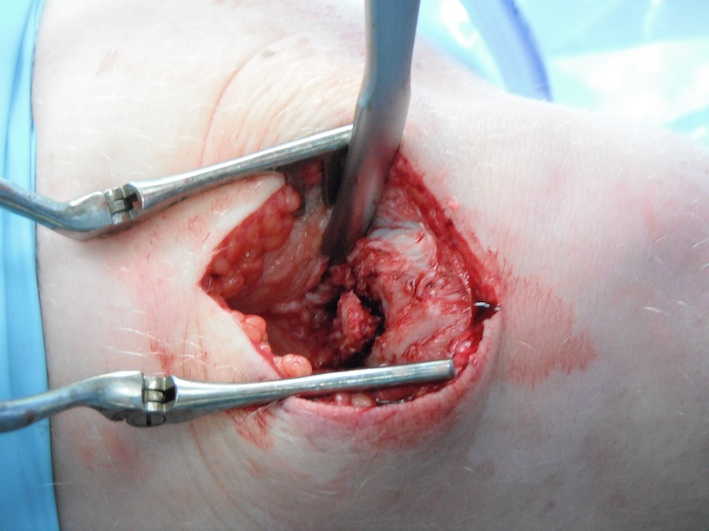
Removal of bipartite patella
A. Open
- easiest
- often need to reattach quadriceps tendon with anchors
B. Arthroscopic