Problem
1. Undulating growth plate / higher rate of growth plate injury
- growth arrest / LLD
- angular deformity
- need to be warned
- require close and careful follow up especially in first 2 years
2. Can be unstable / malunion and shortening very problematic in this area
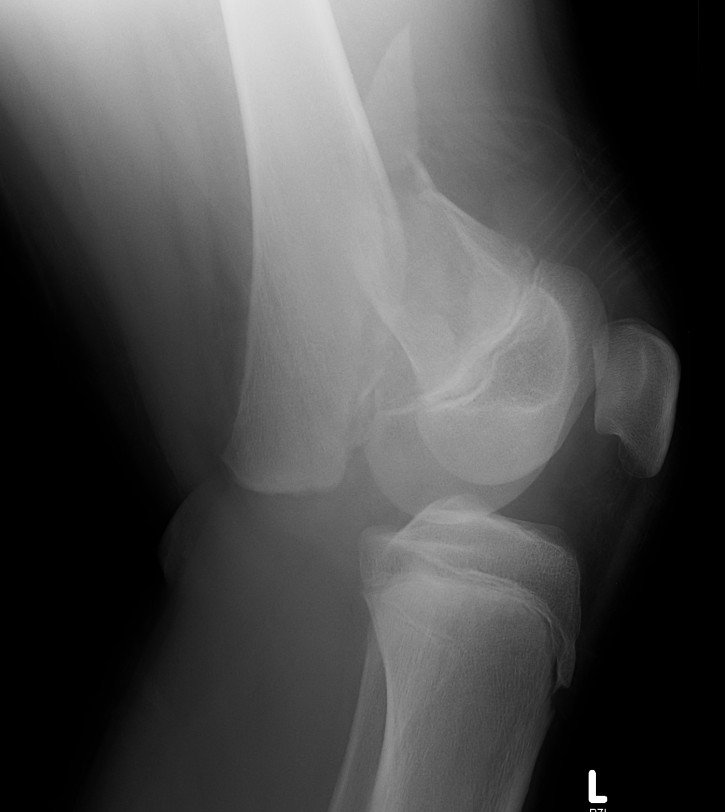
Xray
Salter Harris I


Salter Harris II

Management
Undisplaced
Extension plaster 6 weeks
Displaced
MUA +/- ORIF
Low threshold to ORIF to maintain position
- already have high risk of growth arrest / LLD / angular deformity
- don't wish to deal with malunion / loss of position as well
MUA
Block to reduction
- often medial sided periosteum
- may need small medial subvastus / anteromedial approach
Options
1. Physeal sparing metaphyseal screw in SHII
- good option if Thurston-Holland fragment large enough





2. Smooth transphyseal large K wires / Steinman pin
- SHI
- SHII with small Thurston-Holland fragment
Complications
Complete growth arrest common
Monitor 6 monthly
- plot short and long leg lengths on Mosely chart
- distal femur contributes 9 mm / year
Manage LLD as per predicted difference
- usually contralateral femoral epiphysiodesis if < 5 mm
- may need femoral lengthening / ISKD on maturity if > 5 mm
Partial growth arrest / angular deformity
Moniter closely and investigate any possible growth arrest
CT / MRI
- assess percentage of bony bridge
Bony bridge < 50%
- excision and fat graft
- manage angular deformity with 8 plates / osteotomy
Bony bridge > 50%
- hemi-epiphysiodesis
- may need correction of LLD and angular deformity
- opening wedge femoral osteotomy
