Aetiology

Varies per age group
Trauma
- 60%
Non Accidental Injury
- 15 - 30%
- suspect if non walker / < 1 year
- walking status single best indicator of risk
- paediatric team to investigate
- history taking from parent
- consider metabolic investigations
Osteogenesis Imperfecta / Pathological fracture through cysts
- 10 %
Epidemiology
Bimodal distribution
- peaks at 2-3 and 16-19 years
- younger group from falls
- older group from traffic accidents
Management
Immediate management
Gallows traction
Child 0 - 2 years and < 12 kg


Hamilton- Russell (90/90) traction
- skin traction on lower leg
- place padded sling behind knee to slightly flex
Algorithm
0 - 6 months
- Pavlik harness (neonates with fracture occuring during birth)
- spica
6 months - 4 years
- spica
5 years - 11 years
- length stable - flexible nails
- length unstable - plate (bridge or open)
> 12 years
- length stable - lateral entry nail or TENS (<50kg)
- length unstable - plate
15+
- IMN (lateral or piriformis entry)
Polytrauma/ Soft tissue (any age)
Consider external fixator
Management 0 - 6 months
Aetiology
- difficult delivery
- Osteogenesis imperfecta
- Non accidental injury
Management
A. Pavlik harness
B. Spica
Podeszwa et al. J Pediatr Orthop
- < 1 year child
- 24 in Pavlik compared with 16 in spica
- spica patients tended to be older and heavier
- no difference in outcomes
- 1/3 spica patients had a skin problem
https://www.ncbi.nlm.nih.gov/pubmed/15308892
Management 6 months - 4 years
Goals
- < 15o angulation in all planes
- < 2 cm shortening
Options
1. Double leg spica
2. Single leg spica
Leu et al. JBJS Am 2012
- RCT of 52 pediatric femoral shaft fractures
- single v double leg
- all healed satisfactorily
- single leg more likely to fit into car seats / chairs
https://pubmed.ncbi.nlm.nih.gov/22695973/
Flynn et al. JBJS Am 2011
- walking hip spica v traditional hip spica
- walking spica patients more likely to need wedge correction of mal-alignment
https://pubmed.ncbi.nlm.nih.gov/22159855/

Technique Hip spica
Contra-indication
- abdo injury
- head injury (high spasticity)




Technique
- under GA, on spica table (posterior thorax on post)
- apply stocking net over body and legs
- pressure pads over ASIS
- wool applied
- must have roll of wool over abdomen to give space to breath
- 90/90 sitting spica (knees 90o, hip 90o), hips 30o abduction, 15o ER
Check position under fluoroscopy
- accept <2 cm shortening
- 15o varus / valgus
- 20o flexion / extension
- 10o rotation
Options
- one and one half leg: to knee on contralateral side, include ankle on ipsilateral side
- single-leg spica cast: to ankle on ipsilateral side, no inclusion of contralateral thigh
Post spiceacare
- weekly x-ray for 2 - 4 weeks to detect malalignment
- usually for 6 - 8 weeks depending on age
Postoperative care instructions from Queensland Health
https://www.childrens.health.qld.gov.au/fact-sheet-caring-for-your-child-in-a-hip-spica/
Remodelling





Management 5 - 11 years
Immediate Management
Thomas Splint / Balanced Traction
Technique
- analgesia +/- sedation
- Thomas splint with 2 fingerbreadths diameter clearance around thigh
- cushioning for leg to sit in Thomas splint
- traction bed
- application skin traction to leg, tied to end of Thomas splint, traction by twisting paddlepop stick
- weight off end of Thomas over pulley at end of bed
- this pulls splint away from ischium and peroneum
- rope taken over 2 pulleys at top of bed with weight suspended to elevate Thomas splint from bed
- weight is tied to bed at top to prevent falling onto leg
- splint must be checked 2 x day to prevent pressure areas, needs regular oiling
Definitive management
1. Hip spica
2. Titanium elastic nails (length stable)
3. Plate (length unstable)
Hip spica v TENS
Iman et al Arch Bone Jt Surg 2018
- systematic review of 12 studies and 1012 patients
- patients 2 to 16 years
- hip spica v TENS
- reduced malalignment and faster independent walking with TENS
https://pubmed.ncbi.nlm.nih.gov/29911134/
TENS v Plate
Luo et al. Orthop Surg 2019
- plate v TENS in 51 patients
- average union 2.2 months (range, 1 - 6 months)
- no LLD, rotational or angular deformity in any patient
https://pubmed.ncbi.nlm.nih.gov/31456324/
Flexible nails / Titantium Elastic Nails
Indications
- length stable i.e simple transverse, short oblique, midshaft
- maximum weight up to 50 kg / 12 years old
Contra-indications
- unstable fracture patterns
- > 50 kg

Technique
Synthes surgical technique PDF
Wires
- 30 - 40% of diameter of diaphyseal medullary canal
- i.e. if canal 10 mm wide, use 2 x 4 mm
- 6 - 8 years (3 mm)
- 9 - 11 years (3.5 mm)
- 12 - 14 years (4 mm)
- recommend using 2 wires same diameter to avoid rotational instability
- 3 point bend in wires to get 3 point fixation
- aim for bend at fracture site
Entry points
- medial and lateral insertion
- 1 - 2 cm proximal to distal femoral physis
- oblique entry with awl in direction of nail insertion
- can open with drill bit
- beware proximity of the femoral artery medially
- entry points should be symmetrical
Wire passage
- bend wire for 3 point fixation
- also bend the tip of the wire
- can use F Tool to reduce fracture
- may need small incision and open reduction
- medial entry wire will pass into femoral neck
- lateral entry wire will pass into greater trochanter
- use designated TEN wire cutter to cut wires
- cut off, tap in slightly further, leave 1.5 cm out so can retrieve
- wires that are too prominent can cause bursa / limit flexion / pain / protrude through skin
Vumedi video
https://www.vumedi.com/video/elastic-stable-intramedullary-nailing-for-femoral-shaft-fracture/
Acceptable alignment
- 10o varus / valgus
- 15o flexion / extension
- 15 mm shortening
Post op
- early mobilisation with crutches
- touch weight bearing
- begin full weight bearing with union (typically 6 - 8 weeks)
- remove TENS at 6 months
Complications
Narayanan et a. J Paediatr Orthop 2004
- reported on 79 patients treated with flexible nails
- pain and irritation at insertion site common
- malunion / loss of reduction assocatiated with nails of differing diameters and increased comminution
https://pubmed.ncbi.nlm.nih.gov/15205616/
Titanium v stainless steel flexible nails
Mohamed et al. Europ J Orthop Surg Traumatol 2017
- systematic review of 5 papers
- mixed results
- no obvious difference in malunion or union rates
https://pubmed.ncbi.nlm.nih.gov/24077687/
Plate
Indication
- length unstable fractures (spiral / comminuted)
- very distal or proximal fractures
- patient inability to non weight bear (cognitive impairment / developmental delay)
Options
1. Open Plating

2. Submuscular bridge plating


Technique
- supine on radiolucent table or traction table
- incision 5cm proximal or distal (depending # site)
- blunt dissection to periosteal layer
- run bristow or cobb elevator submuscularly
- 3.5 or 4.5mm LCP plate (depending on patient size and age)
- place plate submuscularly
- use stab incisions to place 3 screws above /below fracture
- sufficient spread
Postop
- TWB / PWB for 6/52 until union
- removal at 6/12
Results
Abott et al. J Paediatr Orthop 2013
- comparison of open v submuscular bridge plating in 79 patients
- increased blood loss in open plating
- increased rotational asymmetry in bridge plating
- no other difference between two groups
https://pubmed.ncbi.nlm.nih.gov/23752149/
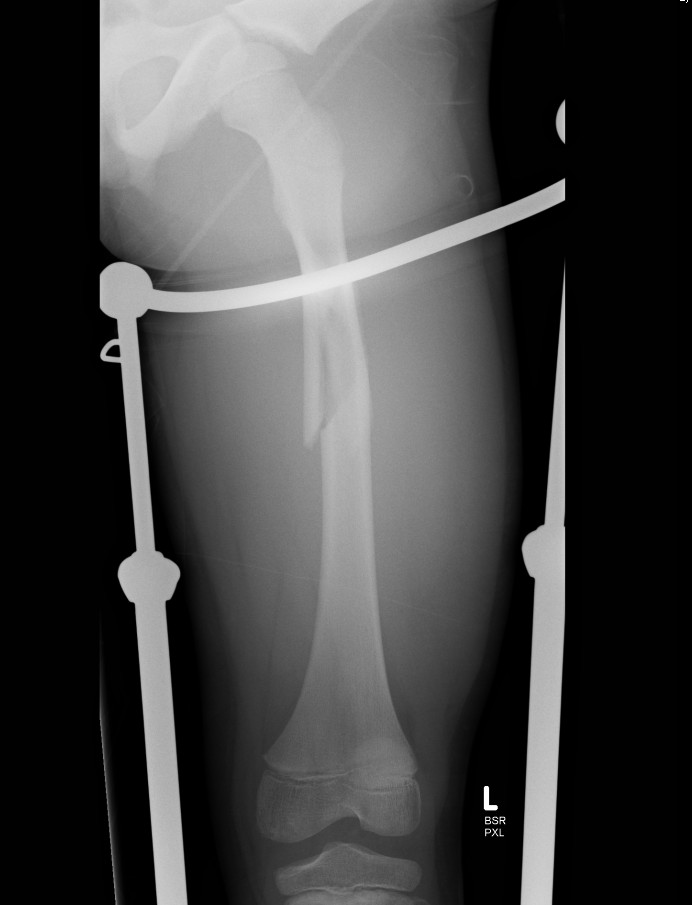
External Fixation
Indication
open wounds as temporary stabiliser
Complications
- pin site infection
- malunion
- refracture post removal
https://www.ncbi.nlm.nih.gov/pubmed/10823615
Management 12 years and over
Issues
1. Less potential to remodel (especially > 10)
2. Usually too heavy for flexible nails
3. Risk of AVN with standard nails
AVN
MacNeil et al. J Paediatr Orthop 2011
- systematic review of risk of AVN after used of rigid locking nails
- piriformis fossa AVN rate 2%
- tip greater trochanter AVN rate 1.4%
- lateral entry / trans-trochanter AVN rate 0%
Acceptable alignment
Varus / valgus 5o
Flexion / extension 10o
Shortening 1 cm
Options
1. Flexible nails
- < 50 kg
2. Plate
Advantage
- very safe option
- avoid growth plates
Disadvantage
- incidence of refracture with plate removal
3. Antegrade Lateral Entry Trans-trochanteric Femoral Nail
Keeler et al. J Paediatr Orthop 2009
- 80 femoral fractures treated with lateral entry femoral nails
- no AVN
- no malunion or nonunion
https://pubmed.ncbi.nlm.nih.gov/19461375/
Synthes surgical technique PDF
4. External Fixation
Management > 15 years old
Standard antegrade nail
- safe
- no risk of AVN
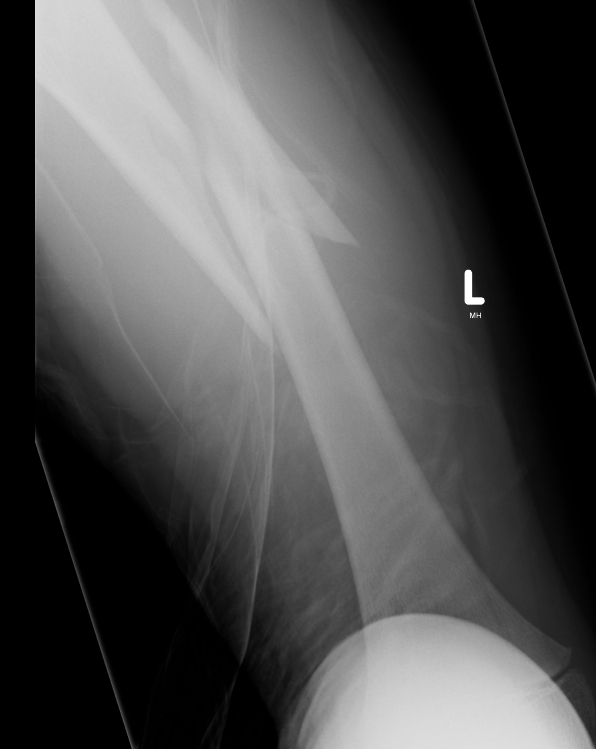
Subtrochanteric fractures
Issues
Non operative treatment rarely indicated in older children as acceptable alignment hard to maintain
- TENS technically more difficult
Options
Plate v TENS
Xu et al. Medicine 2018 PDF
- no difference in outcome between plate and TENS
- plate patients tended to be older and heavier
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6086543/pdf/medi-97-e11568.pdf
