

Epidemiology
Adolescents 12 - 20
Boys > girls
Repetitive overhead or loading actitivities
- throwing athletes / baseball
- gymnastics
- tennis
Kida et al Am J Sports Med 2014
- 2433 adolescent baseball players
- incidence of capitellar OCD on screening was 3.4%
- players with OCD had started baseball earlier and had played longer
DDx
Panner's disease / osteochondrosis
- child 4 - 8 years old
- entire capitellar epiphysis
- ischaemia and necrosis of the capitellum
- followed by regeneration and recalcification
- benign self limiting disease that resolves with rest
Aetiology
Excessive valgus compression across elbow joint
Common throwing sports / gymnastics
- dominant limb
- repetitive overuse
- valgus overload on radiocapitellar joint
- injury to the vascular supply of the subchondral bone
- localized avascular necrosis
Symptoms
Dominant arm / history of over-use
Lateral elbow pain
Limited range of motion
Clicking, grinding, catching, locking - loose bodies
Examination
Tender over lateral aspect elbow
Loss of extension
Radio-capitellar compression test
- active supination and pronation with arm fully extended
Examine MCL
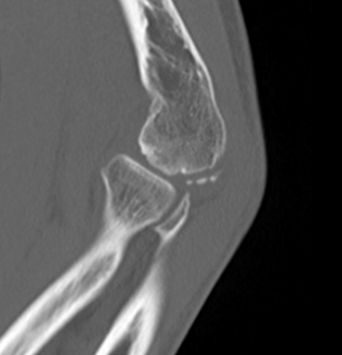
Xray
Kijowski et al Skeletal Radiology 2005
- 50% of capitellar OCD not identified on xray


Localized flattening and translucency Lucency in capitellum
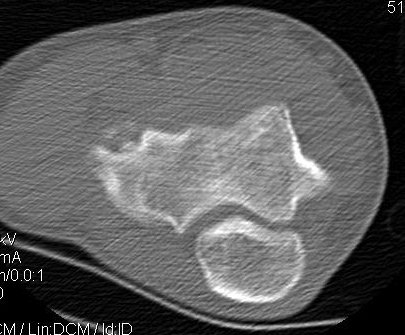
CT


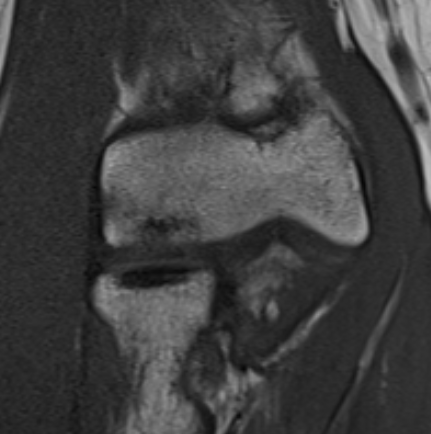
MRI
Fluid interface denotes detachment / instability


MRI Classification
Stable
- cartilage intact
- no fluid behind lesion
Unstable
- cartilage breach
- fluid behind lesion
Bexkens et al Should Elbow 2020
- inter-observer reliability of MRI classification
- acceptable reliability for stable v unstable only
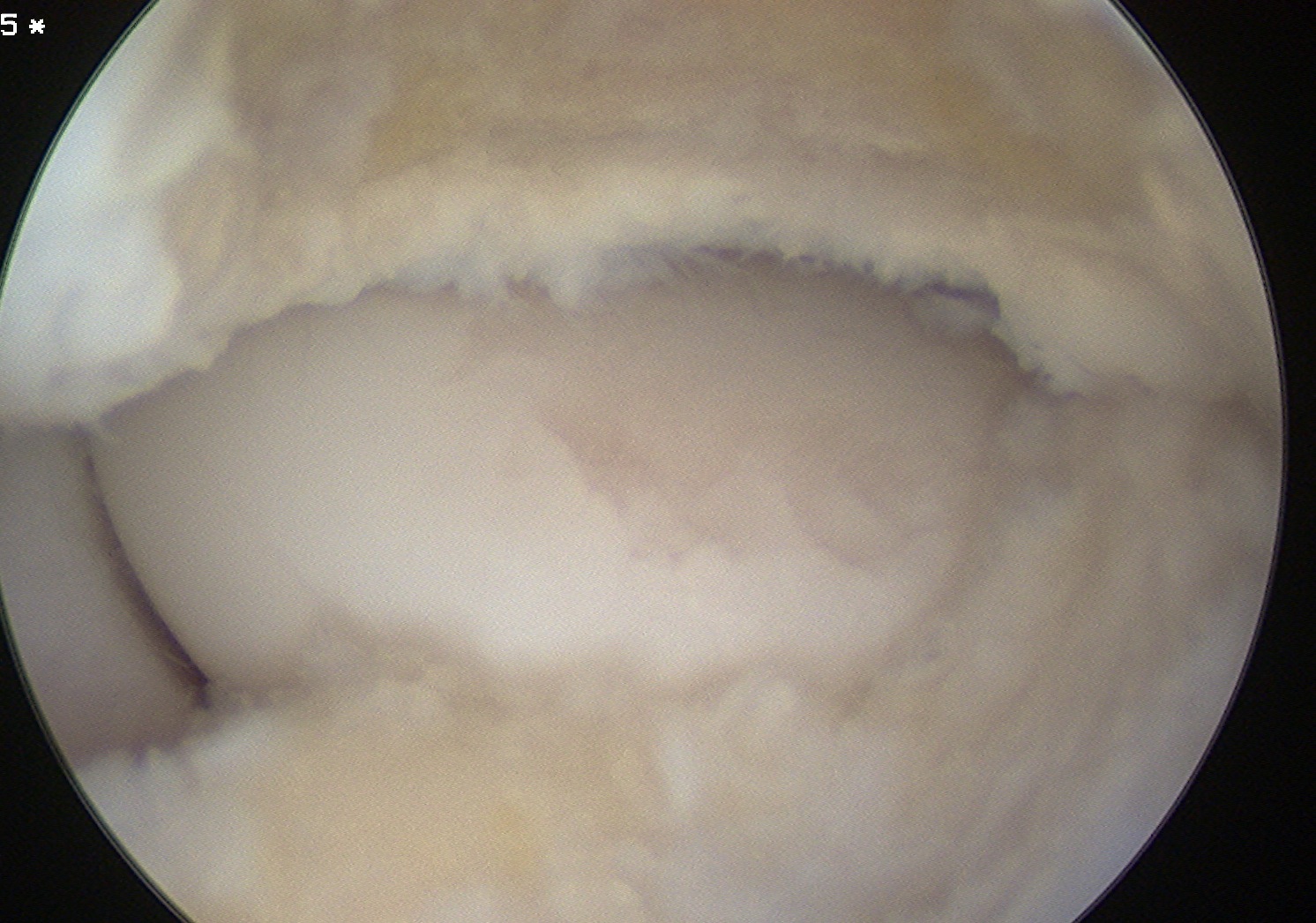
ICRS Arthroscopic Classification
Grade 1: Stable lesion - soft, but cartilage continuous
Grade 2: Partially discontinuous
Grade 3: Complete discontinuity but not dislocated
Grade 4: Empty defect
Locations
Central - lateral wall intact, contained, easier to manage
Lateral wall - uncontained lesion

Lateral capitellar OCD Central contained capitellar OCD
Size
< half diameter radial head
> half diameter radial head
Management
Non operative
Indications
Stable lesion
- intact cartilage
- nil detachment / no synovial fluid behind OCD
Option
Protected ROM
- hinged brace
- attempt to reduce axial load
- nil sports until full ROM
- 3-6 months
Results
Sakata et al Am J Sports Med 2021
- nonoperative treatment of 81 youth baseball players
- return to play 70%
Mihara et al Am J Sports Med 2009
- 39 baseball players mean age 13 years
- cessation of throwing, weights, push ups
- healing of lesion in 16/17 patients with open growth plates
- healing of lesion in 11/22 with closed growth plates
- 25/30 early stage lesions healed
- only 1/9 advanced stage lesions healed
- suggest early surgical intervention in advanced OCD
- recommend surgical intervention if no sign of healing in 3-6 months
Operative
Indications
1. Failure nonoperative treatment
2. Unstable lesions
3. Loose bodies
Outcomes
Westermann et al Orthop J Sports Med 2016
- systematic review of surgical management of capitellar OCD
- 24 studies and 492 patients
- return to sport 64% OCD fixation
- return to sport 71% OCD removal and marrow stimulation
- return to sport 94% osteochondral autograft
Large & salvageable fragments
Options
Drill in situ
Fixation
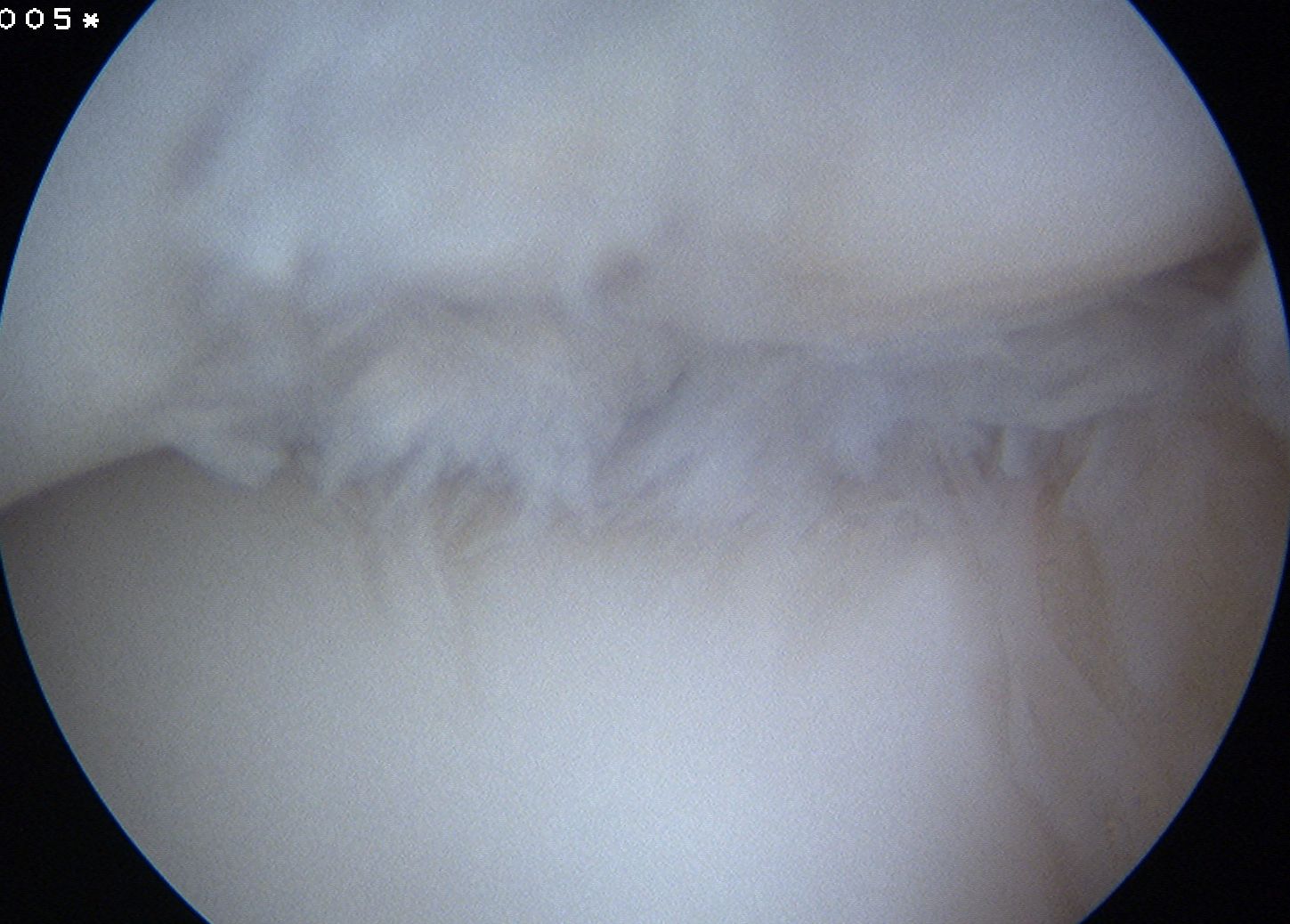
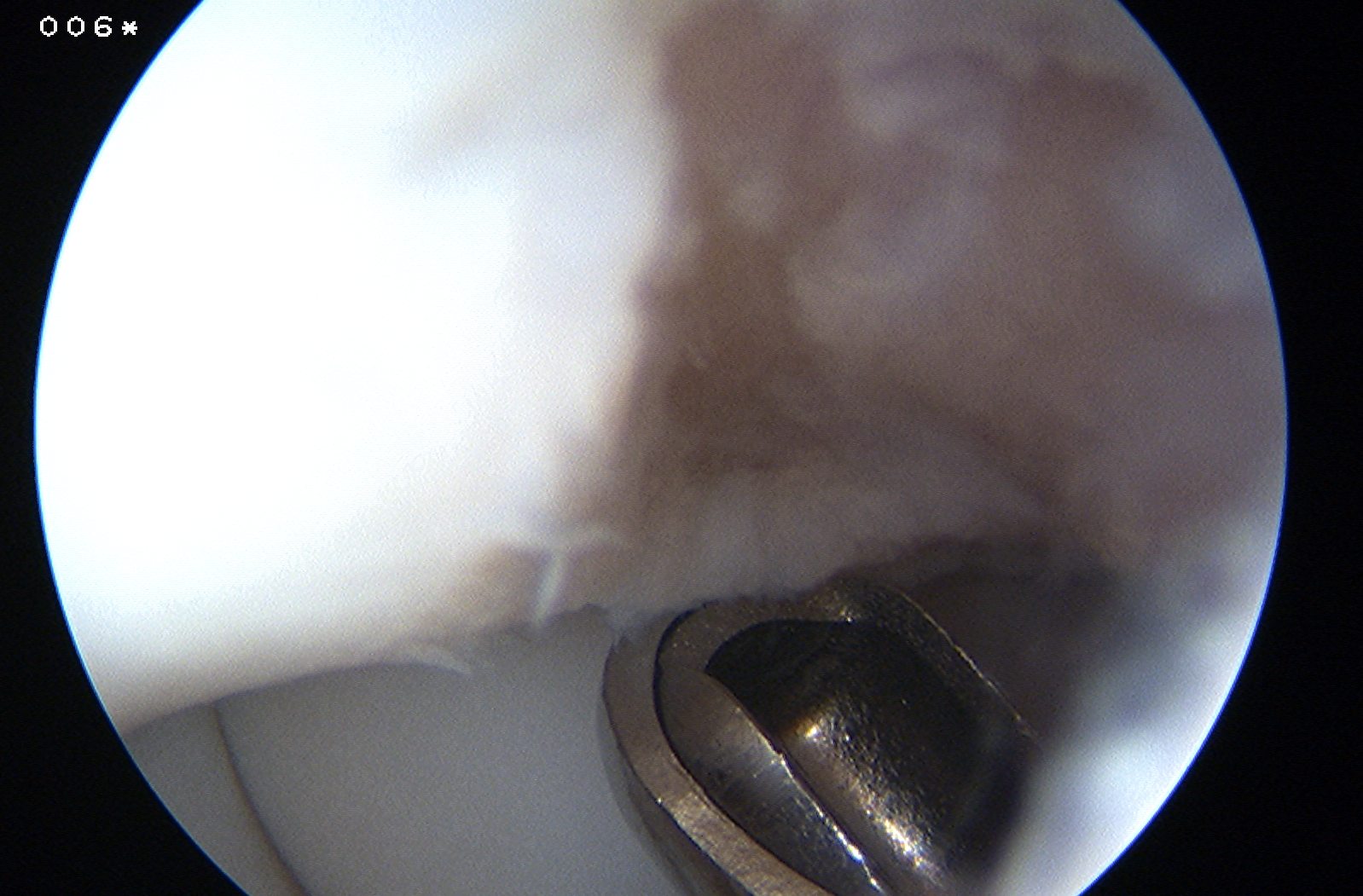
Drill in situ
Indications
Stable lesion
Failed nonoperative treatment
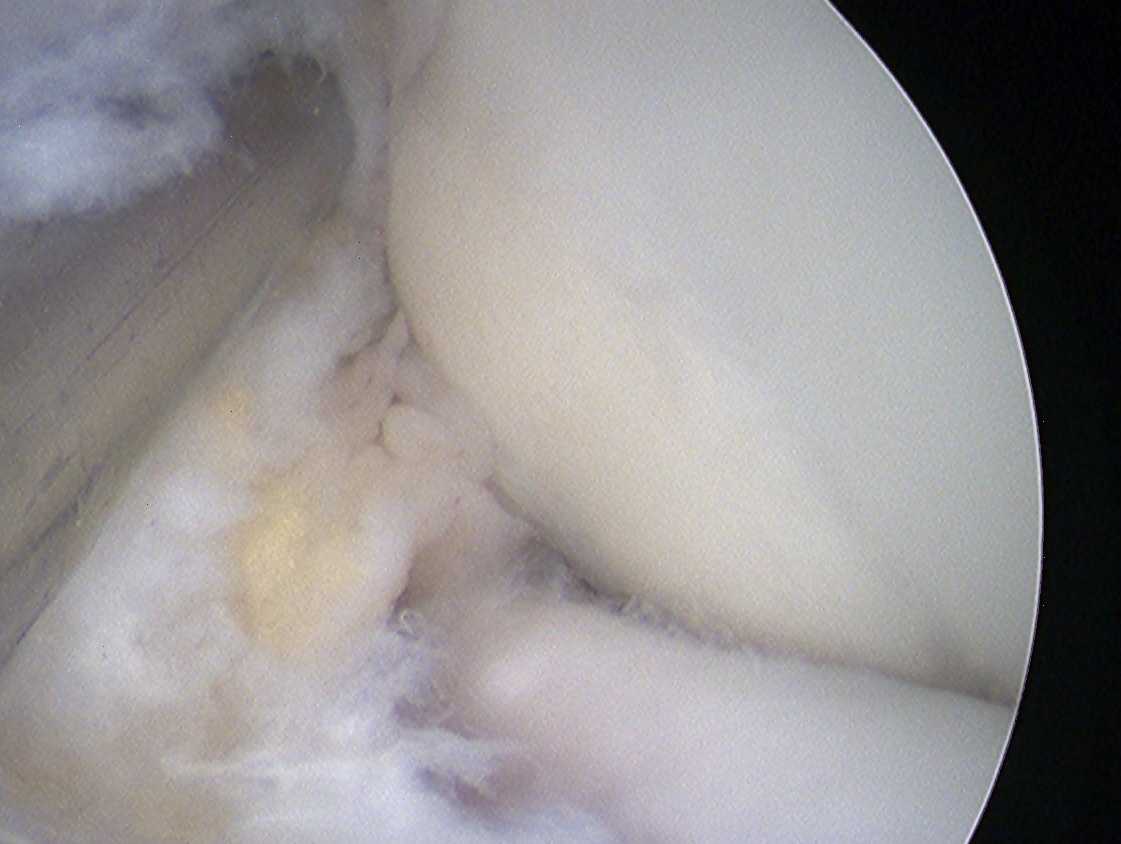
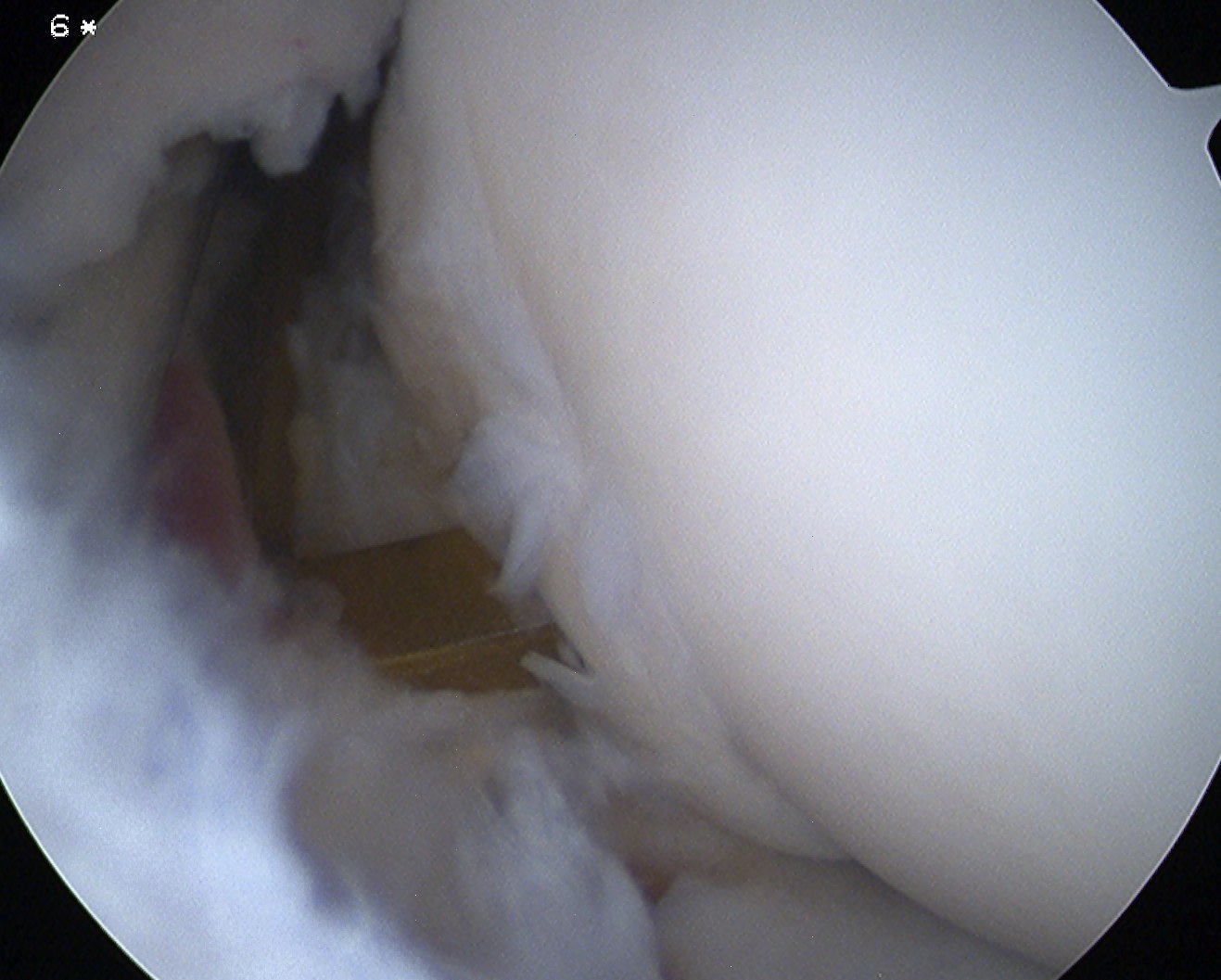
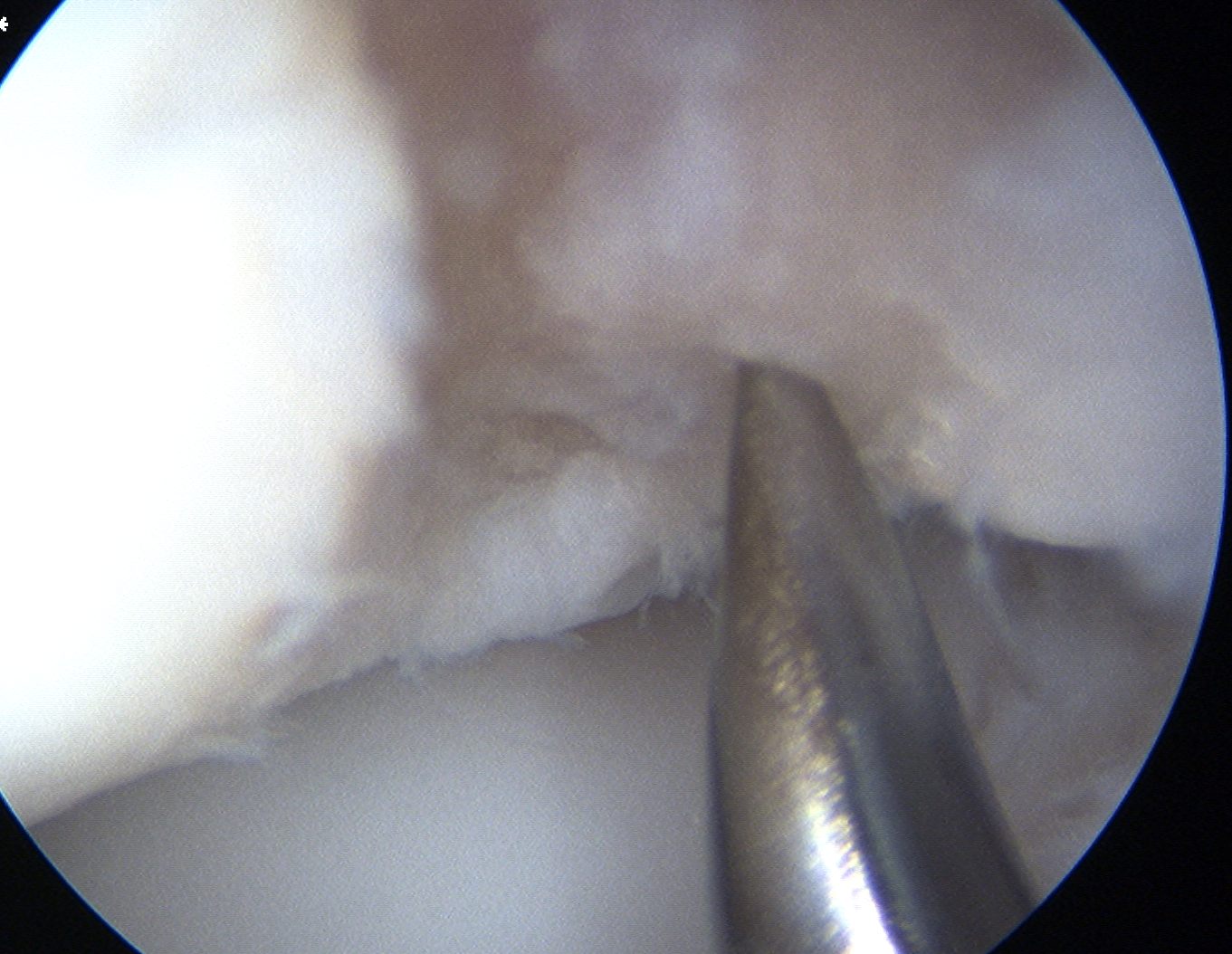
Capitellar OCD viewed via anterior portals, being drilled in retrograde fashion using ACL jig
Arthroscopic technique
1. Anterograde
2. Retrograde using ACL jig
B. Unstable - Fixation
Indications
Acute injury
Large fragment
Minimal bony fragmentation
Technique
Vumedi open capitellar OCD fixation
Outcomes
Hennrikus et al J Paediatr Orthop 2015
- 26 unstable OCD fixed
- 20/26 healed
Small or unsalvageable fragments
Options
Arthroscopic debridement
Arthroscopic debridement + marrow stimulation
Osteochondral autograft
Outcomes
Debridement versus debridement + microfracture
McLaughlin et al Arthros Sports Med Rehab 2021
- systematic review comparing debridement versus debridement + microfracture
- both procedures improved pain, ROM, outcome scores and return to play
- return to play 40 - 100% after debridement
- return to play 55 - 75% after microfracture
- comparable midterm outcomes
Debridement + microfracture versus osteochondral autograft
Westermann et al Orthop J Sports Med 2016
- systematic review of surgical management of capitellar OCD
- 24 studies and 492 patients
- return to sport 71% OCD removal and marrow stimulation
- return to sport 94% osteochondral autograft
Natural history
Ueda et al Orthop J Sports Med 2017
- 38 elbows treated with fragment removal followed for minimum 5 years
- lesions < half radial head had better outcomes than lesions > half radial head
- increased radiological osteoarthritis in group with smaller lesions
Arthroscopic debridement of loose fragments +/- marrow stimulation
Technique
Elbow arthroscopy
Posterior portals
- capitellar OCD viewed by flexing elbow
Arthroscopic technique of debridement and microfracture PDF
Vumedi video capitellar debridement + microfracture
Arthroscopic debridement of loose fragments
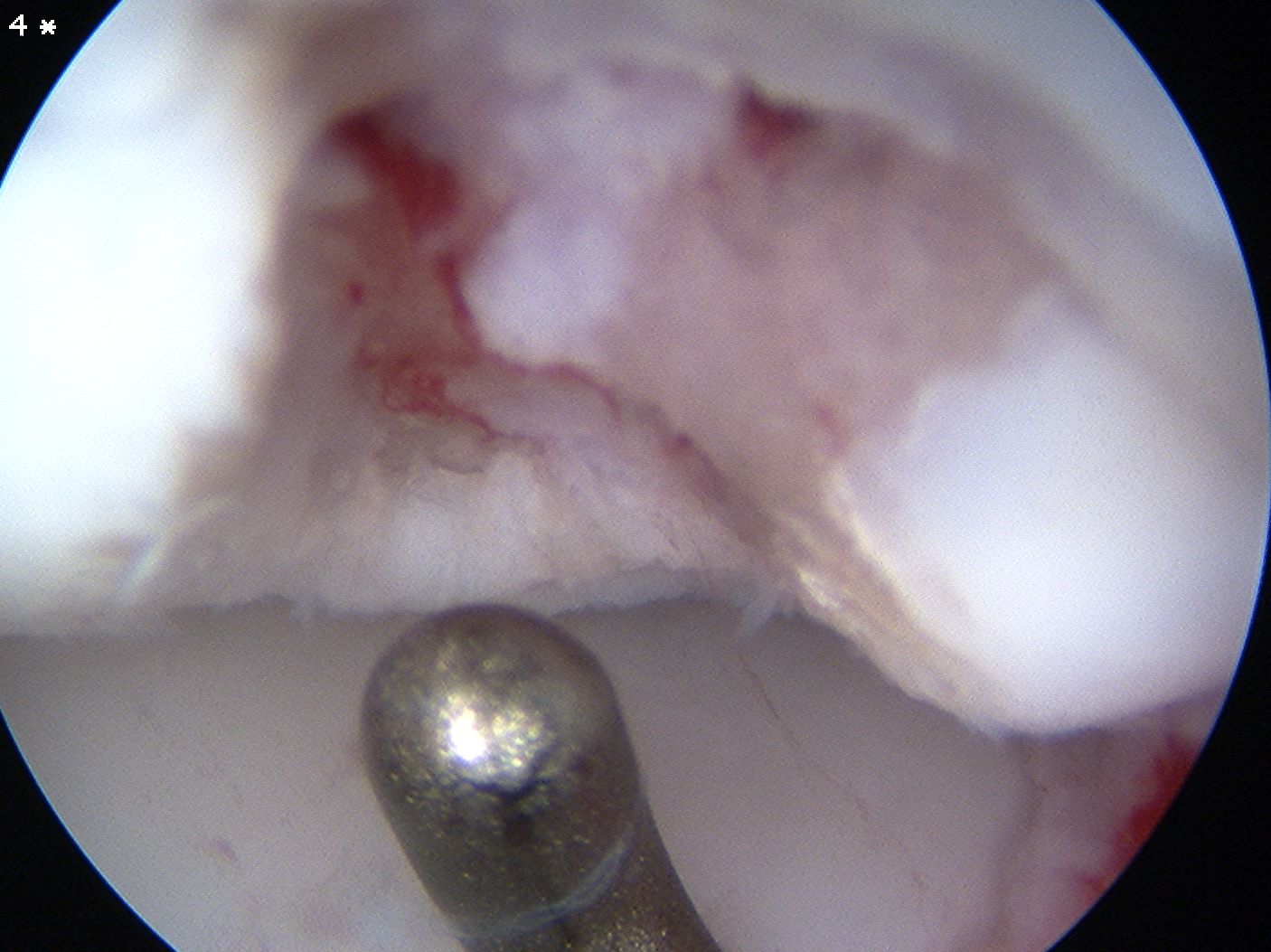
Arthroscopic debridement of loose fragments and microfracture
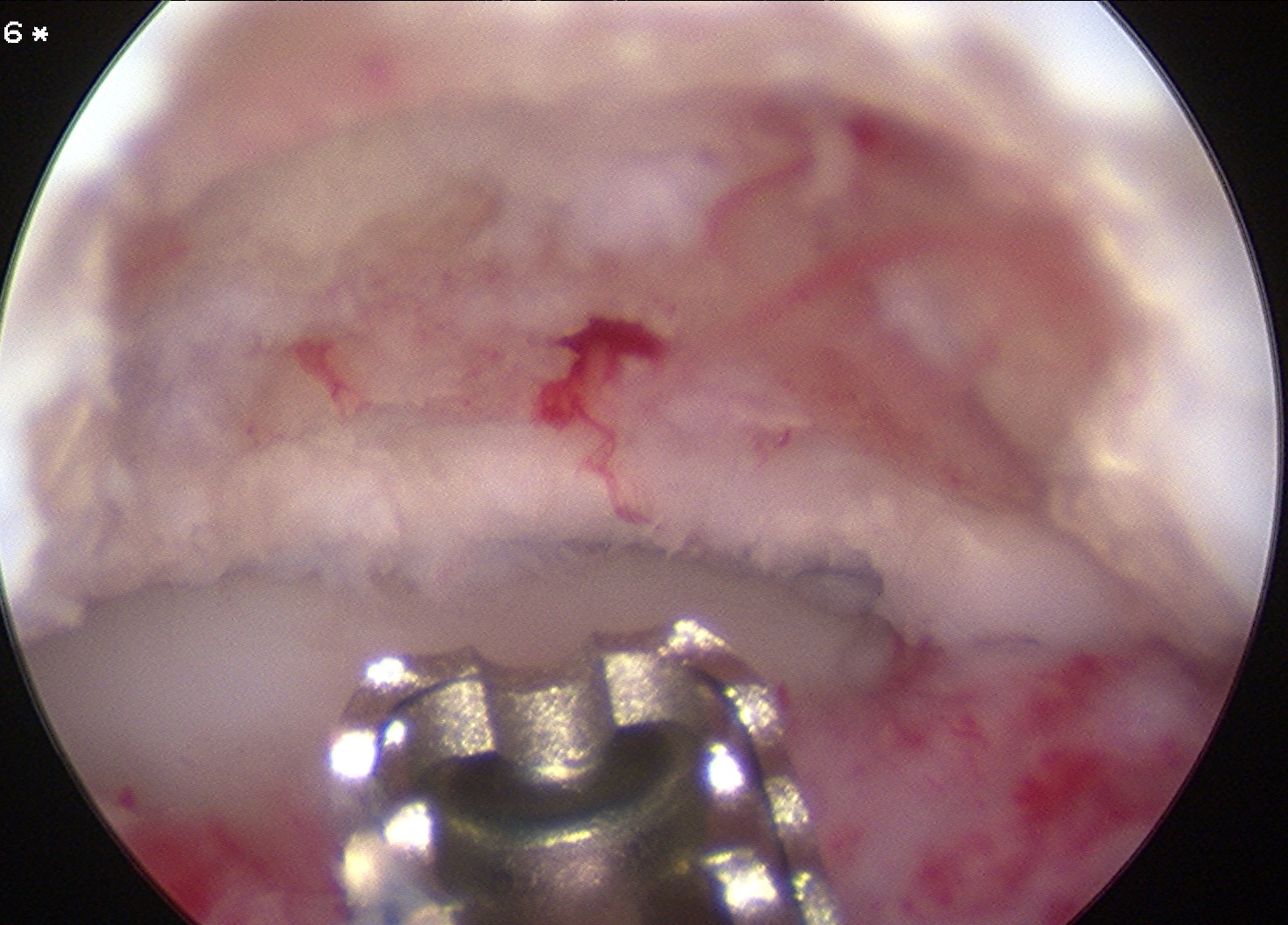
Arthroscopic debridement of loose fragments and abrasionplasty
Capitellar Osteochondral Defects
Options
Osteochondral autograft / mosaicplasty
Osteochondral allograft
MACI
Mosaicplasty
Indications
Unsalvageable OCD
Loose body
Failed arthroscopic debridement and marrow stimulation
Technique
Osteochondral plugs from lateral femoral condyle of knee
Anconeus split approach
Capitellar mosaicplasty surgical technique PDF
AO surgery foundation lateral approach to distal elbow
Outcomes
Maruyama et al Am J Sports Med 2014
- 33 male baseball players mean age 13
- mean defect size 1.5 x 1.5
- plugs from lateral femoral condyle
- 91% no pain
- good improvement in ROM
- 31/33 return to sport at 7 months
Matsuura et al Am J Sports Med 2017
- compared mosaicplasty for 43 central lesions versus 44 lateral lesions
- lateral lesions larger and needed more grafts than central lesions
- better ROM and return to sport in central lesions
- more osteoarthritis with lateral lesions
- no difference in outcomes
