Indications
Poor soft tissues
- prohibit ORIF
Non union
Infected non uniion
Malunion / deformity
Bone loss / bone transport / LLD
Concept
Concept is known as flexible stability
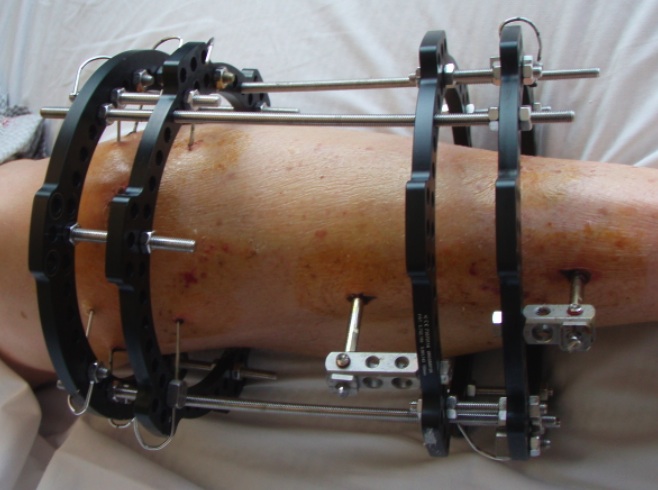
Ilizarov Frame
- controls torsion and shear well
- allows axial compression and controlled micromotion
- this improves bone healing compared to standard external fixation
- tensioned wires tend to loosen over time and improve this situation with further loading
Can compress / lengthen
- lengthen and shorten struts
- allows compression of non union
- allows distraction osteogenesis of corticotomies
Components
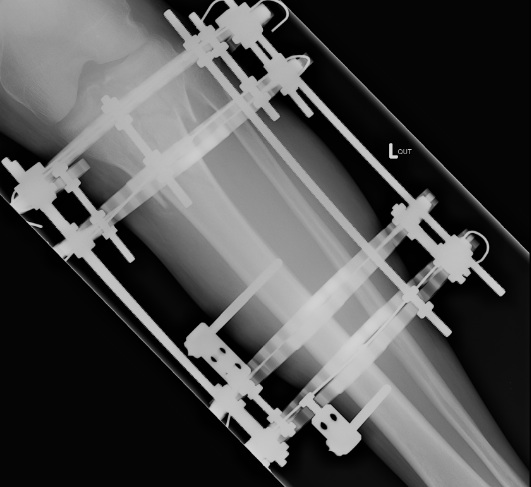
1. High tension wires
- straight or olive
- 90 - 130 kg
- 90o to each other
Olive wires
- used to aid indirect reduction
Tension
- fix one end, tighten the other
Offset wires from rings
- using posts
2. Pins
Use in conjunction to wires
- never at same level as each other to avoid stress riser
- 90o to each other
- 4, 5 or 6 mm
- connected to ring via rancho cubes with centering sleeves
At least 2 planes of wires / half pins in each major bone segment
- very normal to use 1 tensioned wire and two HA coated half pins
- if have 3-4 wires / half pins can remove 1 (i.e. from loosening or infection) without loosing stability of construct
3. Rings
Various sizes
- always need extra room posteriorly
- 2-3cm space to skin circumferentially
- proximal ring open posteriorly to allow flexion
- always 2 level fixation in each level for control
- can be one ring, but wires & half pins above and below
Stability
Techniques
- spread wires
- thicker wires (1.5-1.8)
- increase number of wires
- closer to fracture site
- increase tension
- smaller rings (only 2cm gap)
- olive wires
Wire placement
Anatomic Safe Zones
Aim is to avoid NV structures
- start on side containing critical structures
- push in to bone, drill through cortices
- wet gauze square to stabilise wire
- tap through soft tissue on other side
- muscles on maximus stretch to prevent impalement
- parallel to each other and to ring
- two rings in each segment
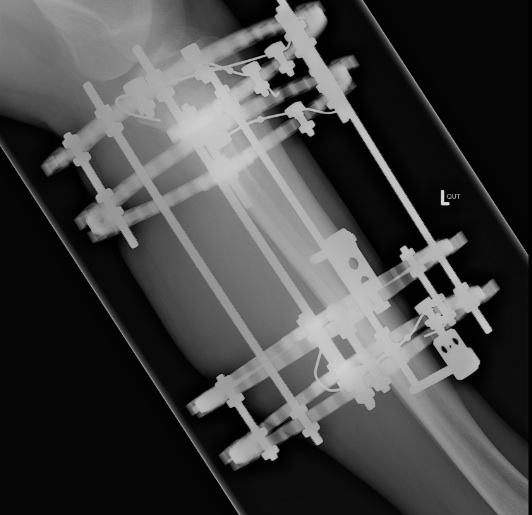
Proximal Tibia
Structures at risk
- CPN
- popliteal artery and tibial nerve
- saphenous nerve
Wires Proximal to TT
- safe arco degrees
- 3 wires
- one wire anterior to fibular head angled anteriorly
- one wire through fibular head straight across posterior tibia
- one wire through medial posterior tibia angled anteriorly
- creates a triangle of bone between wires
- always 10 - 15 mm distal to joint line to avoid proximal joint capsule
- can supplement one wire with two half pins below (HA coated) in the medial cortex
Wires Distal to TT
- safe arc 140o
- not safe to go through fibula
- direct wire transversely

Distal Tibia
Structures at risk
- SPN
- DPN and anterior tibial artery
- posterior tibial artery and tibial nerve
- saphenous nerve
Wires
- one wire through fibula head angled anteriorly
- one through posterior medial tibia, angled anteriorly
- one straight across
- again supplement with half pins above and below


Complications
Good pin site care is aided by avoiding loosening
- pin site complications are frequently related to loosening
Pin site infection
Reduce by
- subcutaneous (don't go through muscle)
- away from zone of injury
- adequate skin incisions
- predrill to avoid thermal necrosis
- manually insert pins
- HA coating
- regular pin site cleaning
- early oral Abx
New self drilling pins are designed for motorised insertion
- avoids problem of "wobble " with hand insertion
HA coating
- improves fixation and decreases infection / loosening
Tapered pins
- increase preload and decrease loosening
- cannot back the pin up or become loose
Pin site care
- motion of skin is most deleterious
- leave a compressive dressing intact for 1 week
- simple daily showers with soap sufficient
Pin site infection
- must remove if loose
- oral Abx
- more regular cleaning
- topical bactroban (mupirocin)
Soft tissue impalement
Effects
- loss of motion
- scarring
Prevention
- check ROM intraoperatively
- position joint in neutral
Late Malunion / Refracture
Dynamise frame / remove struts
- allow patient to weight bear in frame
- should be non painful