Acetabular Fracture
Etiology
Press-fit component
- under-reaming
- excessive medial reaming
Incidence
- CT of 585 THA
- occult acetabular fractures in 8%
- most common superolateral acetabulum
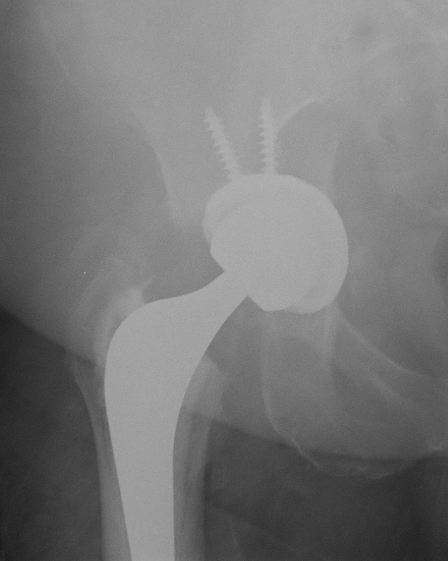
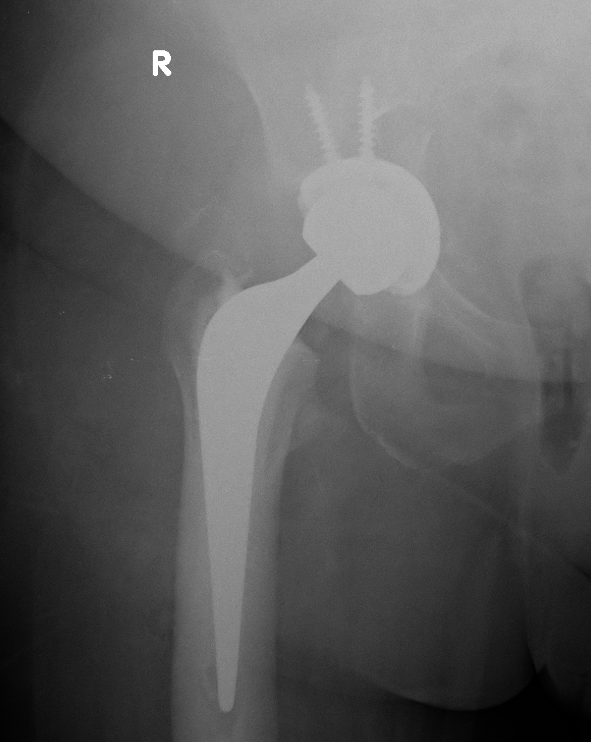
Callous from occult intra-operative acetabular fracture
Prevention
Don't under-ream >1mm
Osteoporotic bone - line to line reaming
Undisplaced fracture + stable cup
Managment
Acetabular screws
Touch weight bear for period
Results
Yamamuro et al Arch Orthop Trauma Surg 2022
- 38 patients with occult acetabular fracture during THA
- no loosening
- 100% 10 year survival
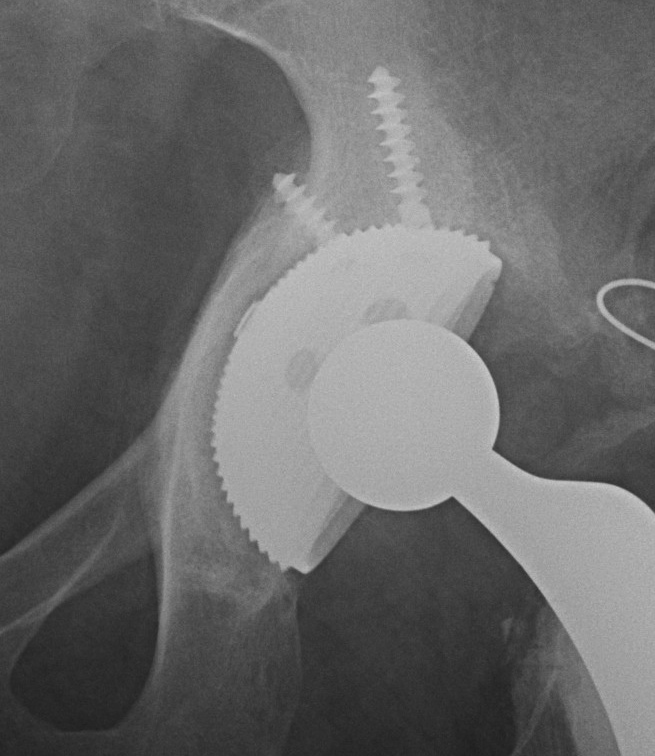
Displaced fracture
Management
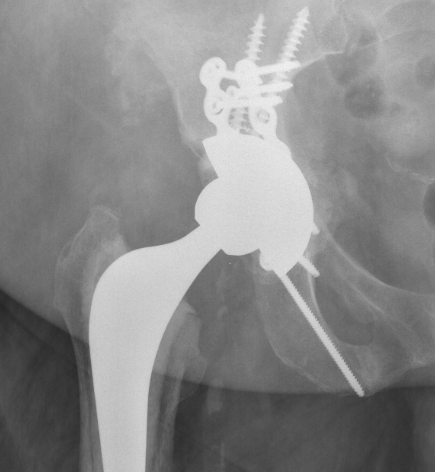
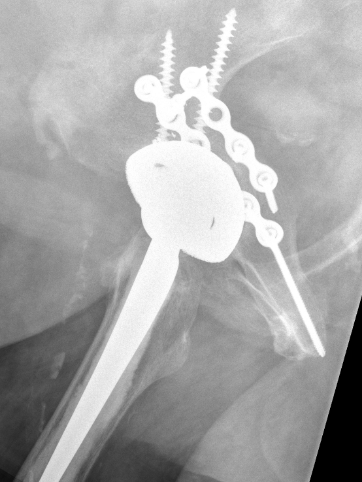
- plate posterior column if fractured
- screw fixation anterior column
- additional screws in cup +/- cage
- touch weight bear for period
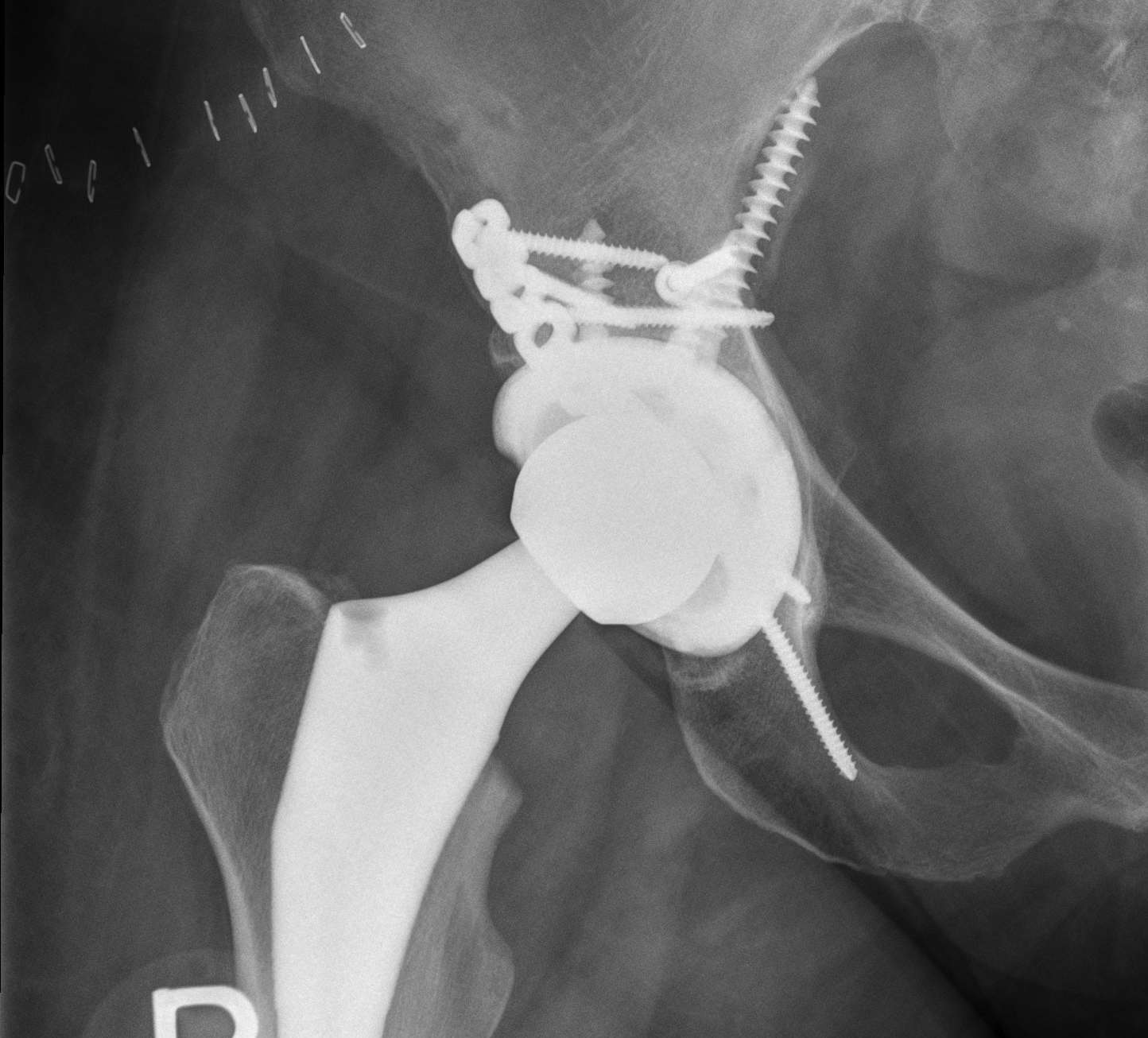
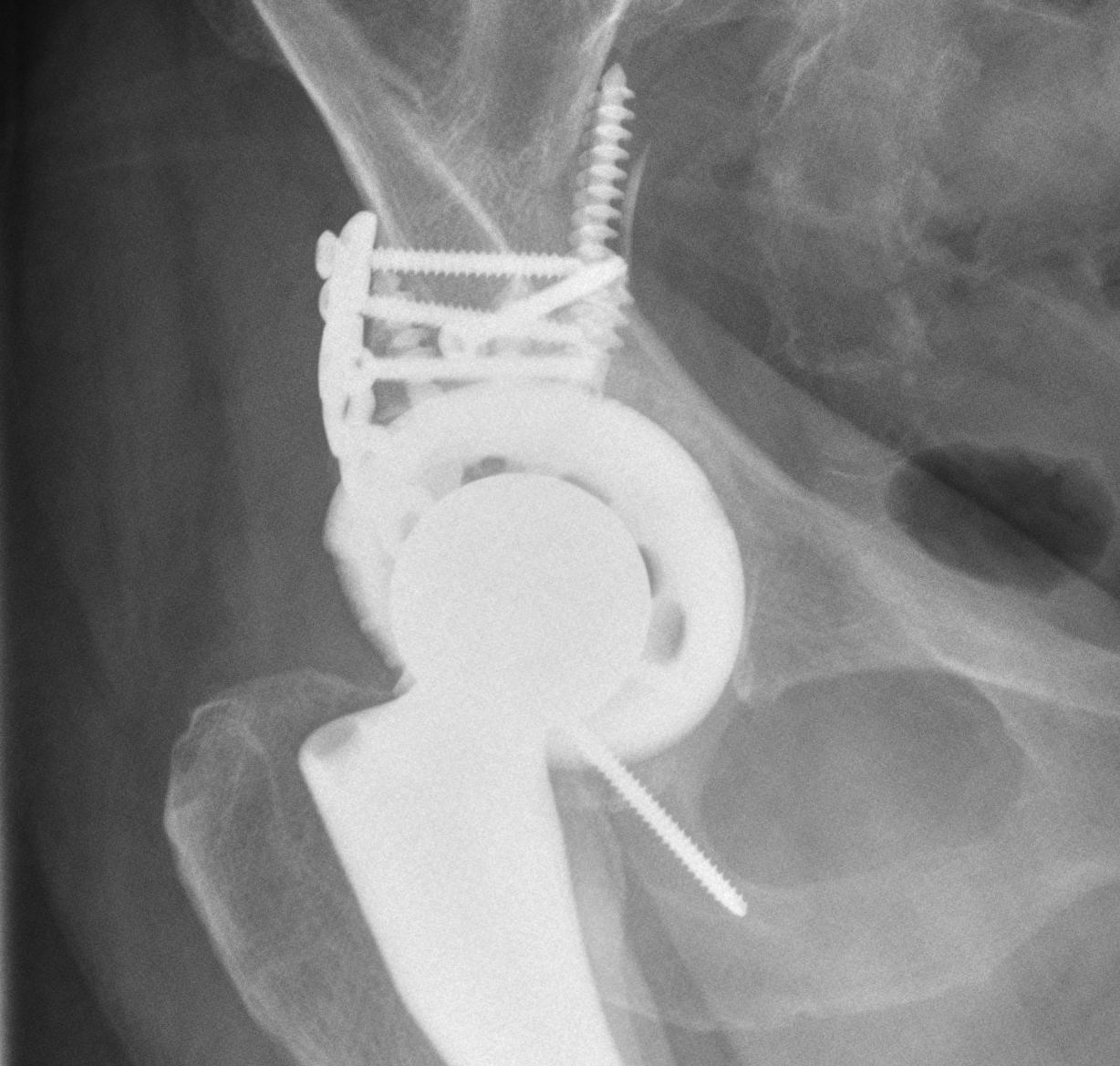
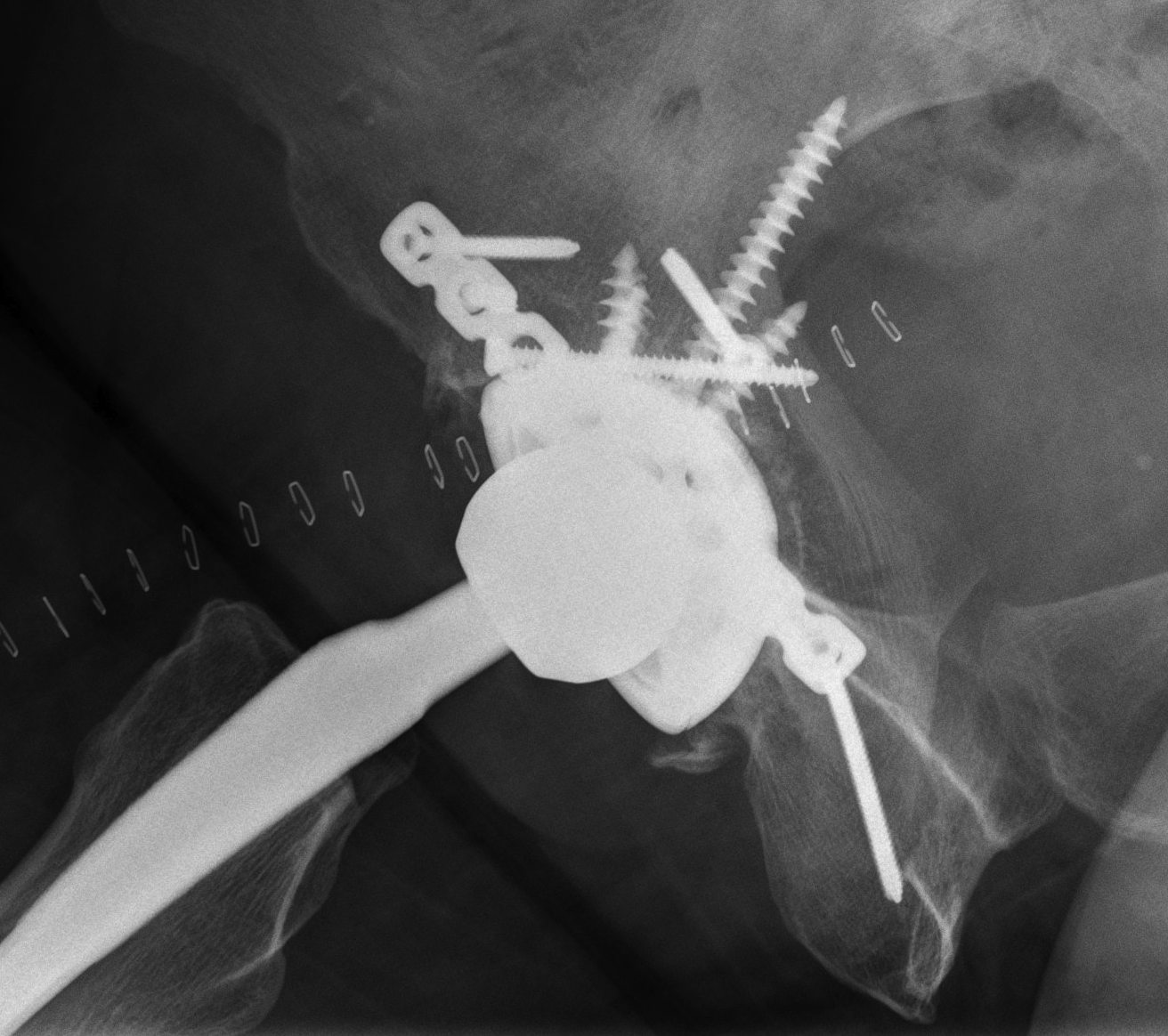
Intra-operative acetabular fracture
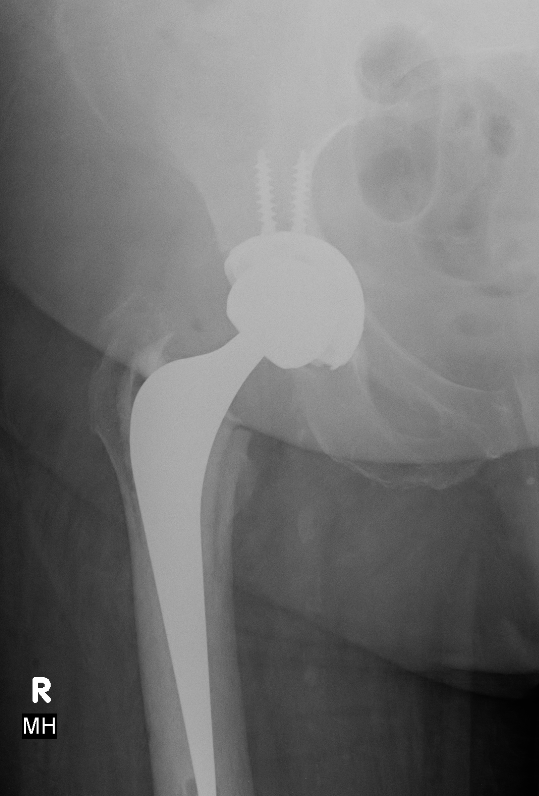

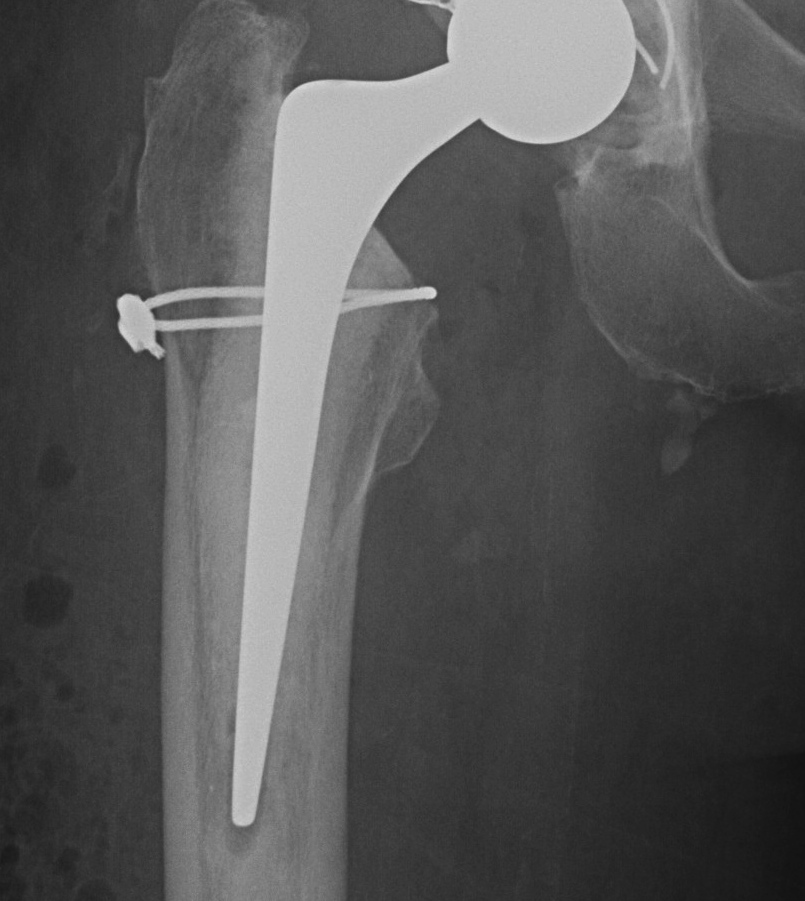
Postoperative acetabular fracture treated with double posterior plating
Femoral Fracture


Risk factors
Uncemented, press fit implants
Elderly females
Osteoporosis
Revision
Timing
Hip dislocation
- careful with rotation
- ensure full releases
Implant insertion
Management
Cerclage wires
+/- bypass fracture with longer stem
+/- plate
