Principle

Correct alignment and soft tissue balancing
- two of the most important aspects of successful TKR
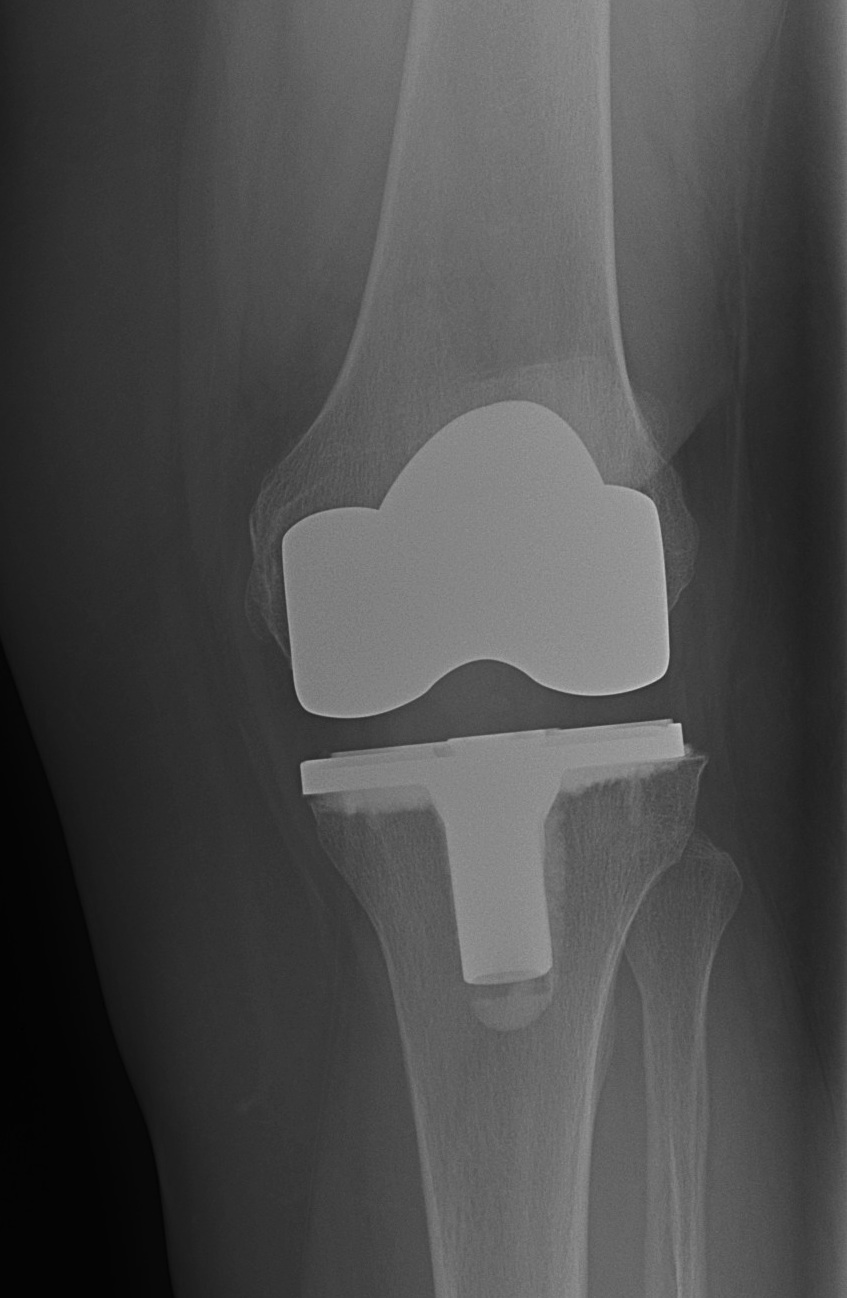
Technical Goals
1. Restoration of mechanical alignment
- forces of the leg pass through the centre of the hip, knee and ankle
- allows optimal load share through medial and lateral sides of the prosthesis
2. Preservation / restoration of joint line
3. Balanced ligaments
4. Maintaining or restoring normal Q angle
Malalignment
Post operative mechanical limb axis within a range of 180 +/- 3o
- associated with lower rates of aseptic loosening
Rand and Coventry 1988
- 90% 10 year survival 180 +/- 4o
- 71-73% when deviation > 4o
Creates a net varus or valgus moment
- excessive stress on one side of the knee
- excessive wear
- early failure


Axis
1. Coronal Plane
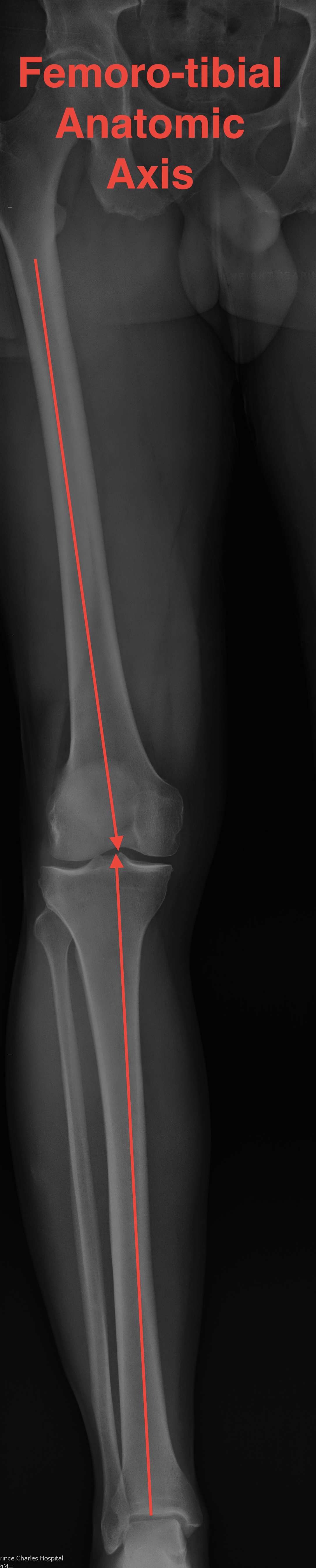
Mechanical Femorotibial axis
- centre of femoral head to medial tibial spine
- medial tibial spine to centre ankle
- should be a straight line 180o +/- 3o
Anatomic Femorotibial axis
- anatomic axis of femur and tibia
- should be 6o +/-3o
Anatomical Axis Femur (AAF)
- centre of femoral medullary canal to midpoint whiteside's axis
- usually exits at intercondylar notch
- entry point for IM rod of femoral jigo
Mechanical Axis Femur (MAF)
- centre of femoral head to centre of knee joint
Valgus cut angle
- angle between femoral and mechanical axis
- LL standing AP
- usually between 5 and 7o
- if cut the distal femur at the valgus cut angle, will place the femoral prosthesis mechanically neutral

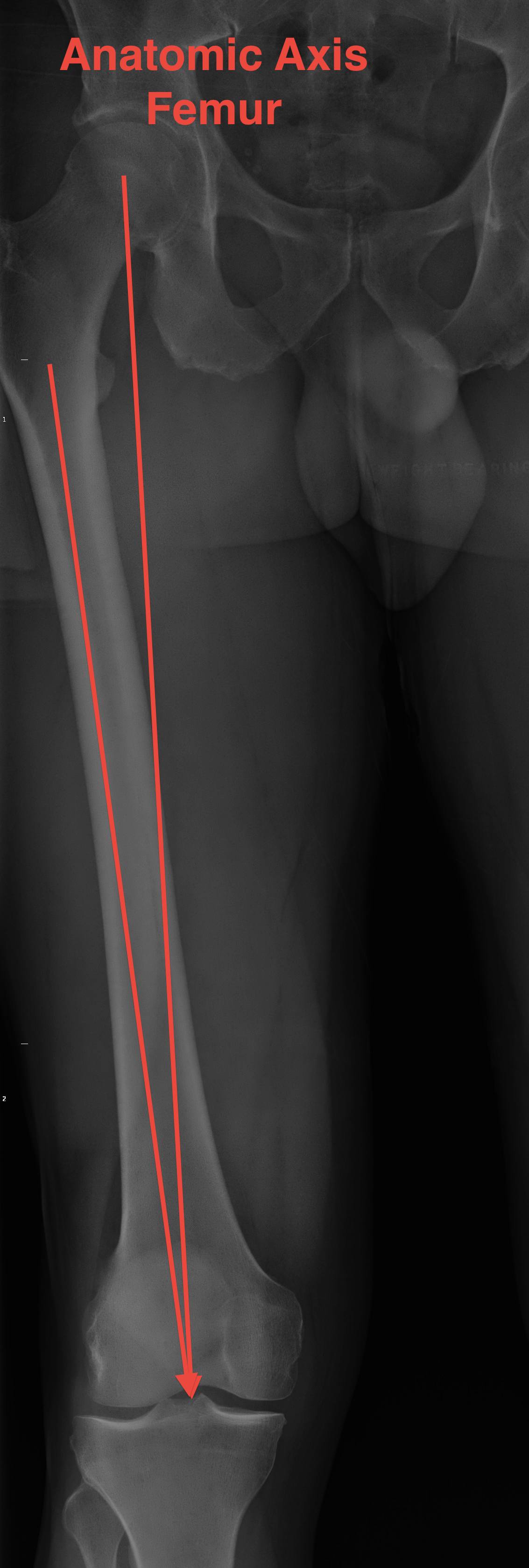
Short patients - > 7o
Very tall patients - < 5o
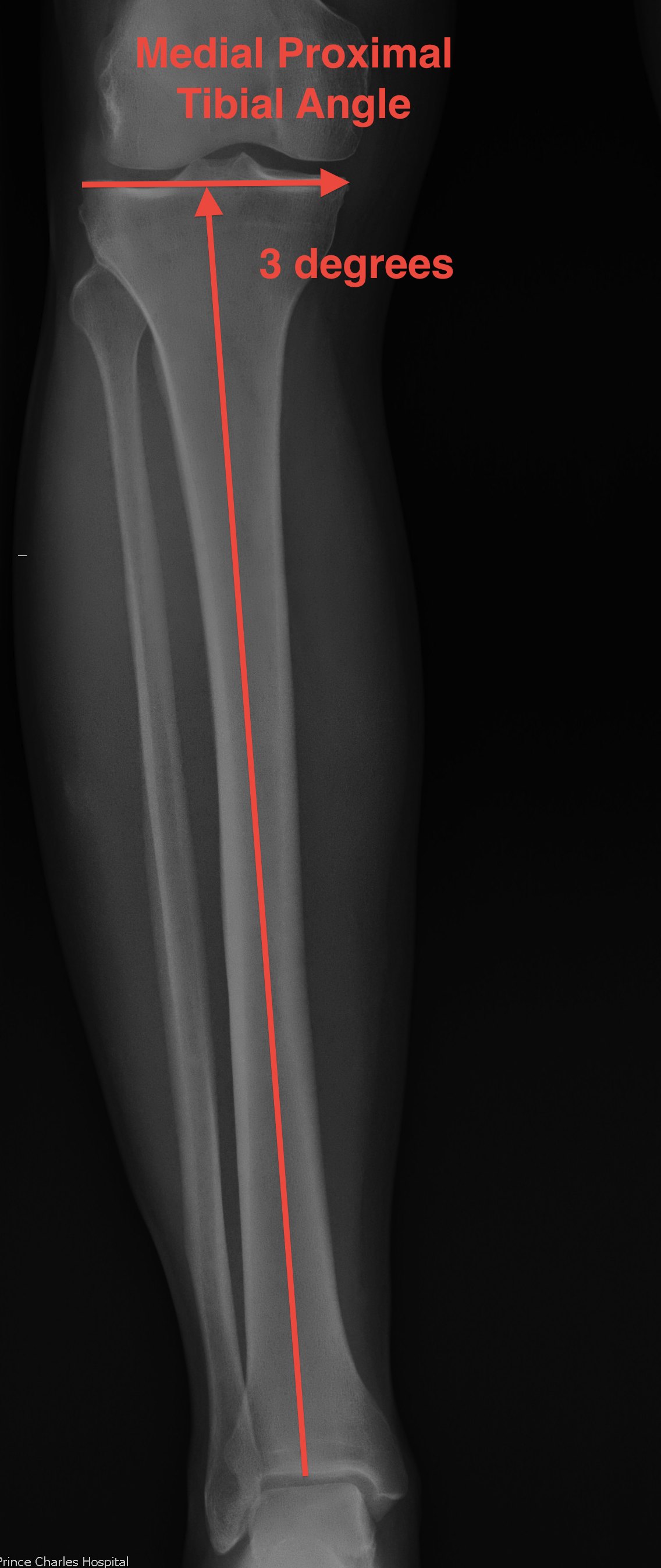
Anatomical axis Tibia (AAT)
- centre of tibia to proximal joint line
- normally 3o varus
- medial proximal tibial angle 87˚
Mechanical Axis Tibial (MAT)
- centre of tibial spines to centre of weight bearing axis of the distal tibia
- usually same as AAT
- except with traumatic or congenital bowing

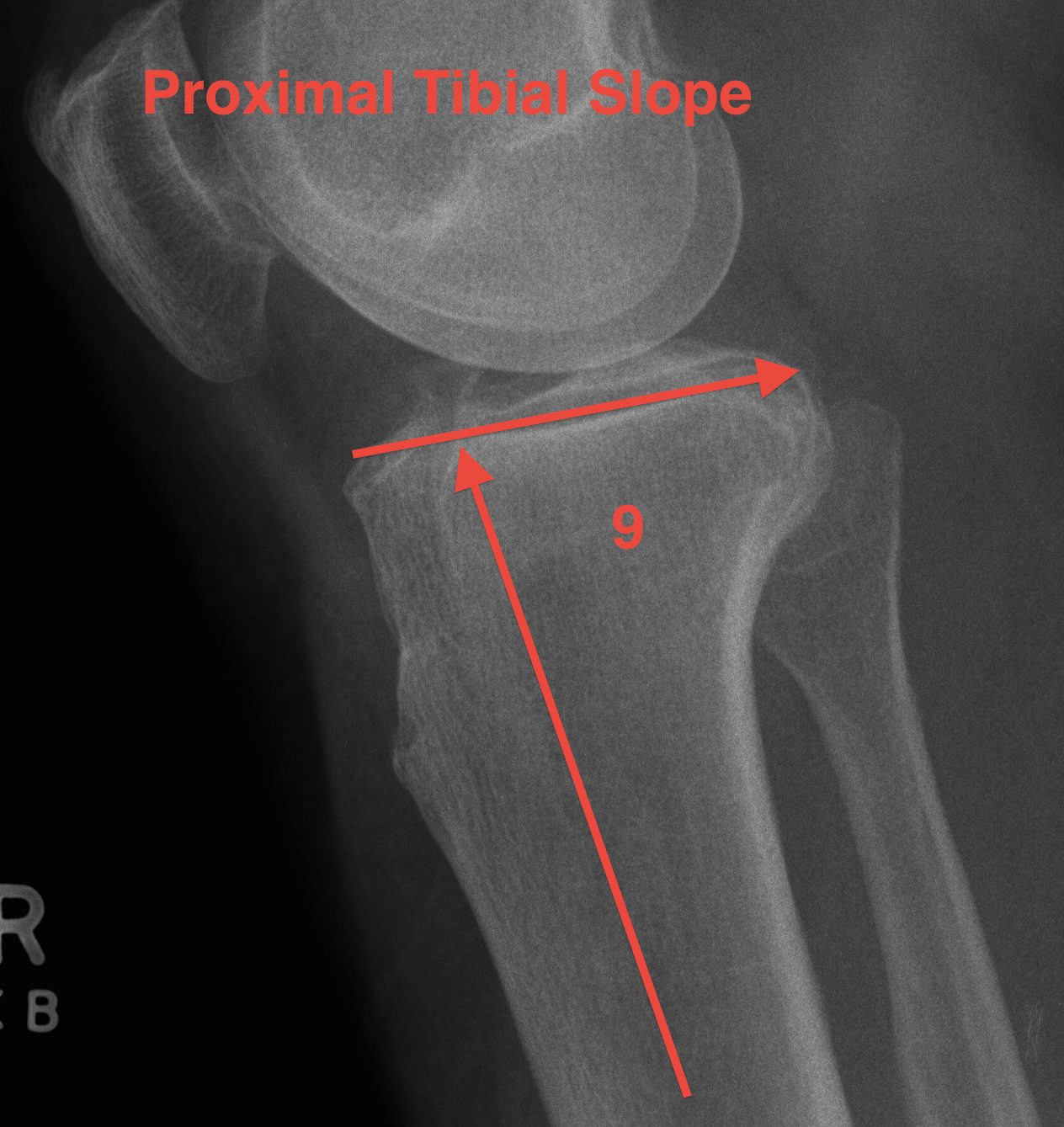
2. Sagittal Plane
Posterior slope
- proximal tibia 10° posterior slope in sagittal plane
- in the knee this is reduced by the menisci
3. Femoral Rotation
Preferred rotational alignment of the femur is slight external rotation to the neutral axis
2 reasons
1. Restores Q angle and normal patella tracking
2. Balances the flexion gap
- proximal tibia normally in slight varus of 3o
- the tibial cut is made at 90o
- perpendicular to the mechanical axis
- the distal femoral cut is made 90o to the axis
- these two cuts match up in extension
- to maintain a symmetric flexion gap, the femoral component must be externally rotated by the same amount
- in flexion, the tibia has been ER by 3o to 90
- must do so to the femur
- allows balanced ligaments in flexion
Methods of establishing neutral rotational axis of the femur
1. Leo's Line / Whiteside's axis
- AP axis of the femur
- line running down the centre of the trochlea to the top of the intercondylar notch
- centre of trochlea groove to centre intercondylar notch
- AP cut is made perpendicular to this axis
2. Epicondylar axis
- only landmark available in revision
- place femoral component parallel to the epicondylar axis
- AP cut is made parallel to this axis
3. Posterior condylar axis
- line connecting bottom of medial and lateral posterior condyles
- AP cut is made in 3o of external rotation to this line
Effects Internal rotation Femur
1. Unequal flexion extension gaps
- alters relative dimensions of posterior condyles in flexion
- tight medially
- loose laterally
- discomfort
- limited flexion
- accelerated poly wear
2. Lateral patella tracking
3. Anterior medial femoral notching
4. Tibial Rotation
Internal rotation of tibial component
- relative external rotation of tibial tubercle
- increase the Q angle
Alignment and Resection Methods
Most systems use Classic Alignment & Matched Resection
- cut tibia and femur perpendicular to MA
- ER femur 3°
- balance soft tissues
Two alignment methods
1. Classic method alignment
Insall
- matching mal-alignments by 3°
- joint lines cut perpendicular to MA
- tibia cut in neutral / over-resect lateral tibial plateau
- femoral cut in 3° varus
Problem
- in flexion the lateral flexion gap is too large & trapezoidal
Overcome by ER femur 3°
2. Anatomic alignment
Technique
- cut 9° to the femoral shaft
- corrects for 3° malalignment in flexion gap
- have to use in conjunction with Matched Resection Method
Two resection methods
1. Matched resection method
Technique
1. Bony resection first
2. Ligament balancing
Advantage
- avoids problems of excessive bone resection to balance contracted capsule in Flex / Ext Gap Method
- the intact femoral condyles is the distal reference femur
- posterior LFC is the AP Femoral Reference
- preserves the joint line relative to the collaterals
2. Flexion extension gap resection method
Insall
- cut tibia perpendicular to mechanical alignment
- automatically ER femoral component 3° by IR femur 3° with Tensioner in flexion gap
Advantage
- again matched mal-alignments
- usually gives good result if not severe deformity / contracture
Problems
A. Capsule contracture causes excessive bone resection
- carefully address this prior
- post capsule contracture leads to excessive distal femoral resection
- are stable in extension, unstable in flexion
B. Mid flexion instability can result
C. The joint line is not fixed, its position is relative
