Epidemiology
Up to 40% of rotational ankle injuries involve posterior malleolus
Isolated posterior malleolar fractures
- Volkmann fractures
- uncommon
- 1% of all ankle fractures
Issues
| Joint stability | Syndesmosis | Functional outcomes |
|---|---|---|
|
Large fragments - 30 - 40% Posterior joint subluxation |
PITFL attachment to posterolateral fragment Syndesmotic instability |
Evidence of improved outcomes with operative fixation Articular steps Increased contact pressures |
 |
 |
 |
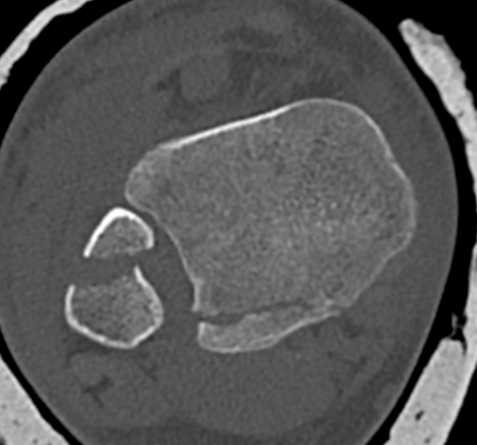
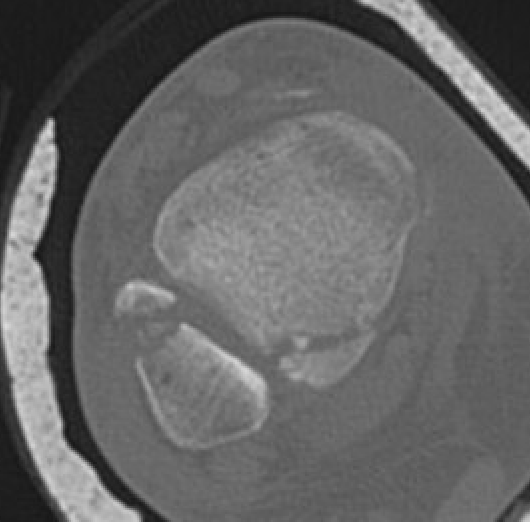
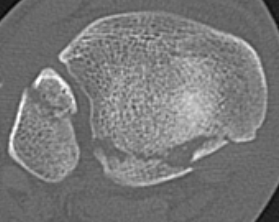
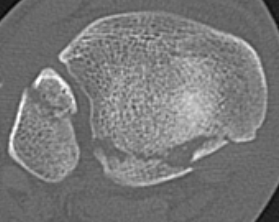
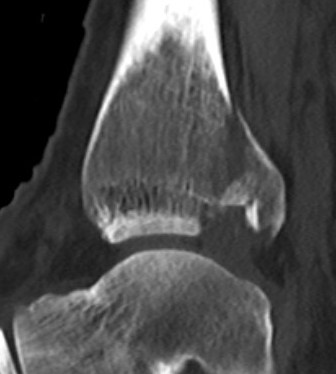
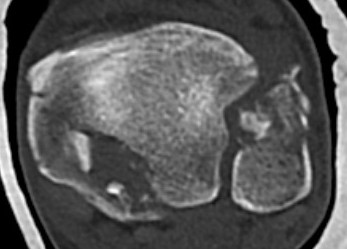
Mason and Malloy Classification
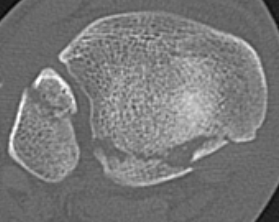
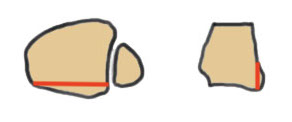
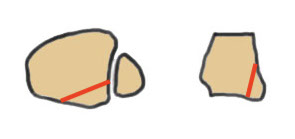
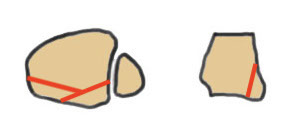
CT scan critical to classify and guide treatment / approach
| Type I | Type IIA | Type IIB | Type III |
|---|---|---|---|
| Avulsion of the PITFL |
Posterolateral fragment Volkmann fracture |
Posteromedial & posterolateral fragments Volkmann plus secondary fracture line |
Large coronal plane fragment Plafond fracture |
 |
 |
 |
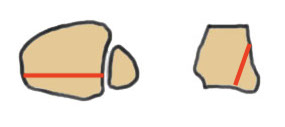 |
 |
 |
 |
 |
Management
Reduction
Large fragments can be very unstable
Occasionally external fixation is required




Operative management
Indications
1. Large fragment / ankle joint subluxation
2. Articular incongruency / articular step
3. Syndesmotic involvement


Dislocated ankle joint with large posterior malleolus


Articular incongruency

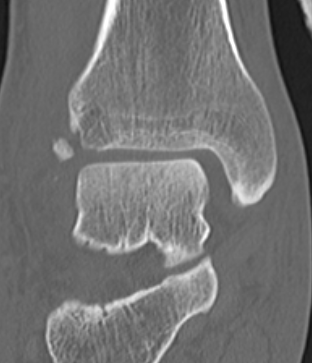
Posterior malleolus and syndesmotic injury
Options
1. Indirect reduction and AP screws - small fragment that can be reduced
2. Posterolateral approach - posterolateral fragment
3. Posteromedial approach - posteromedial fragment
Results
Operative versus non operative management
Miksch et al Foot Ankle Int 2023
- systematic review operative versus non operative treatment of posterior malleolus fractures
- evidence for superior functional outcomes of operative treatment
Outcome
van Hoof et al Foot Ankle Int 2015
- 131 ankle fractures with posterior malleolus fracture
- OA associated with larger fragments and articular step > 1 mm
Indirect versus direct reduction
Haws et al Foot Ankle Orthop 2023
- 120 posterior malleolus ORIF
- malreduction defined as > 2 mm articular step off
- indirection reduction: 24%
- open reduction: 8%
Blocks to reduction
Aamir et al Eur J Orthop Surg Traumatol 2024
- retrospective review
- 22% incidence of tibialis posterior tendon blocking reduction with posterior malleolar fractures
Indirect reduction and AP screws


Posterolateral approach
Prone position
Advantage
- better visualisation
- gravity assists posterior malleolus reduction
- ORIF posterior malleolus and fibula
Disadvantage
- harder to access medial malleolus
Lateral position
Advantage
- place on sandbag
- ORIF posterior malleolus and fibula
- can then deflate sandbag to approach medial malleolus with patient supine
Disadvantage
- poorer view of posterior malleolus

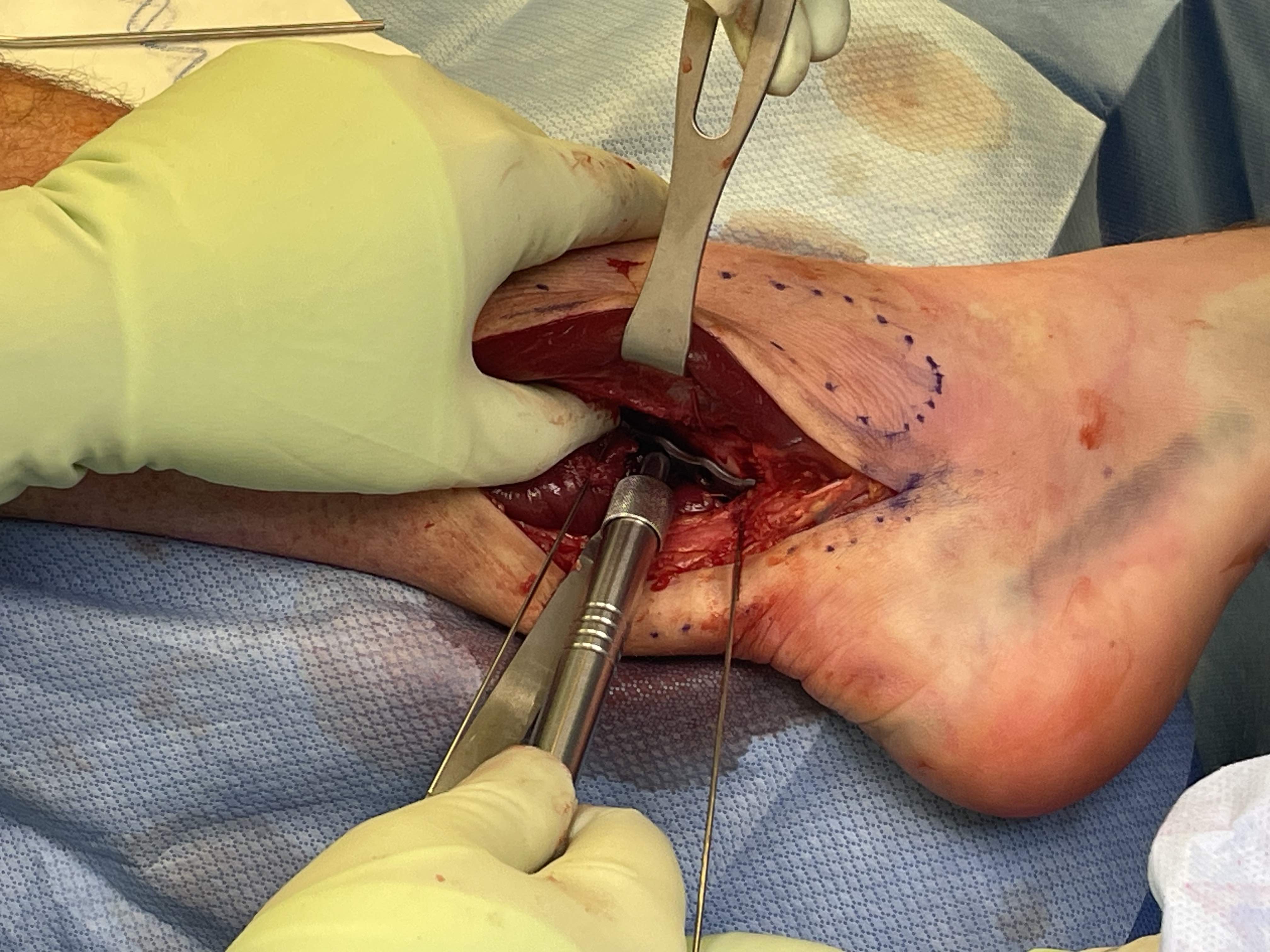

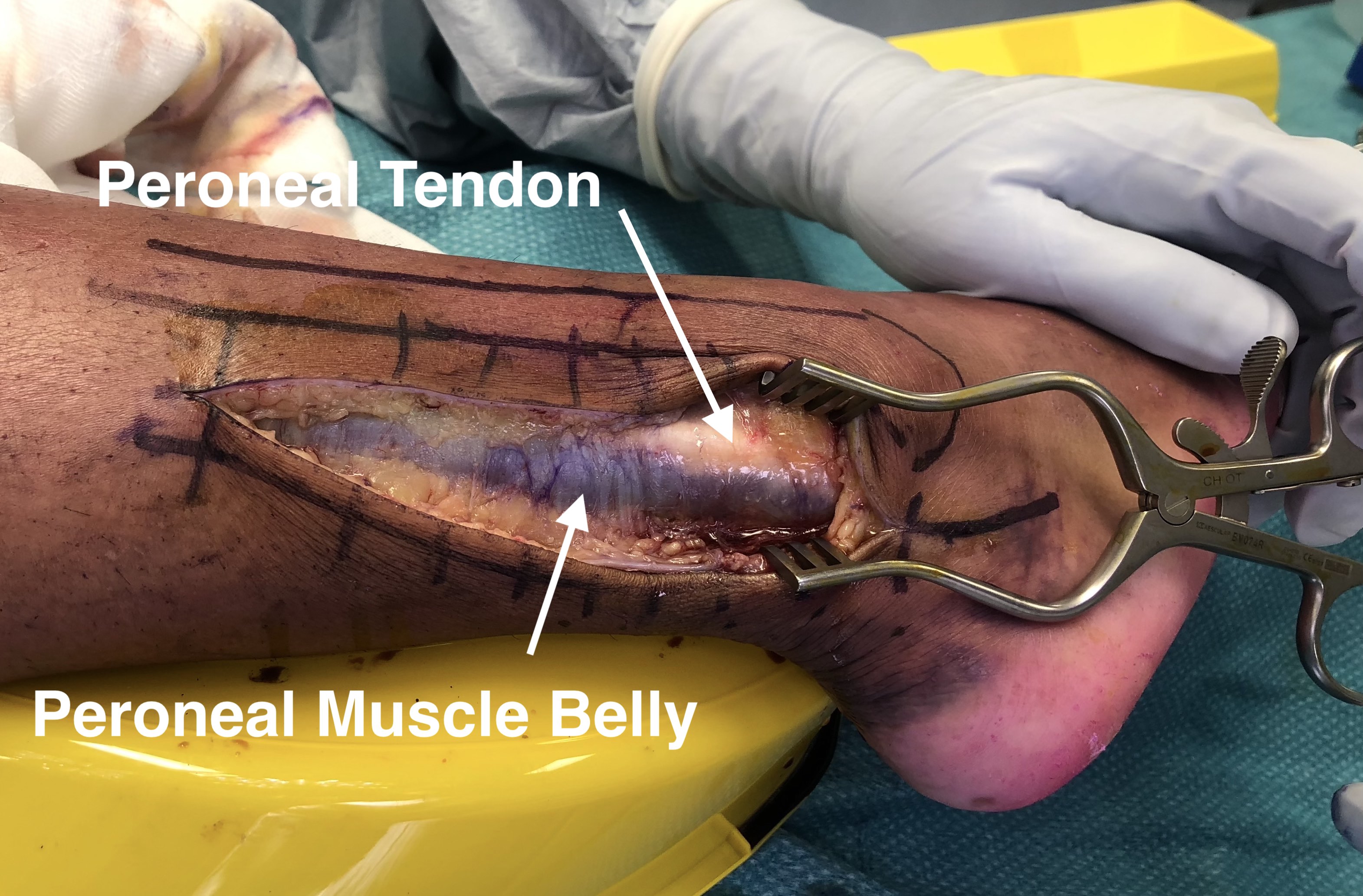
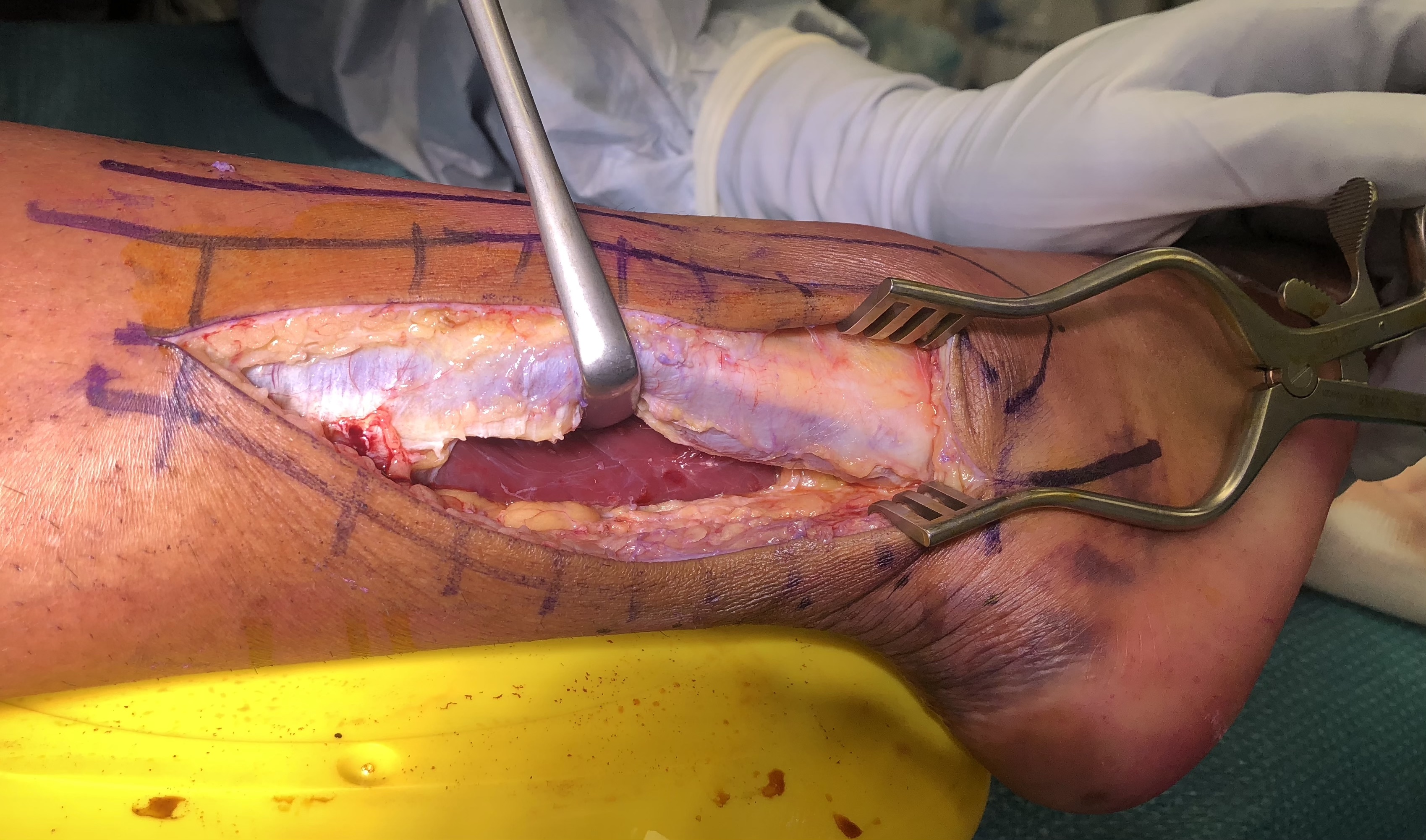
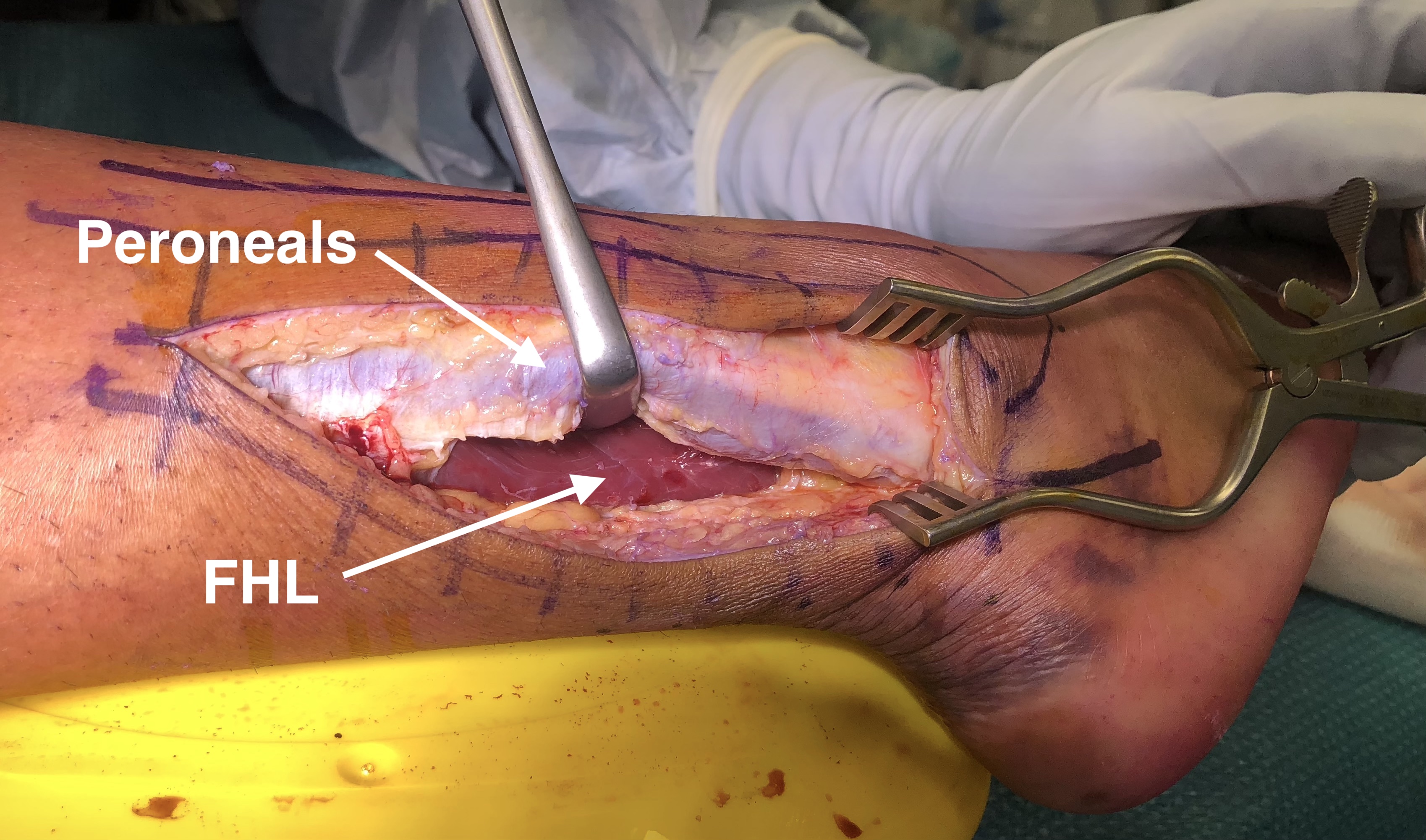
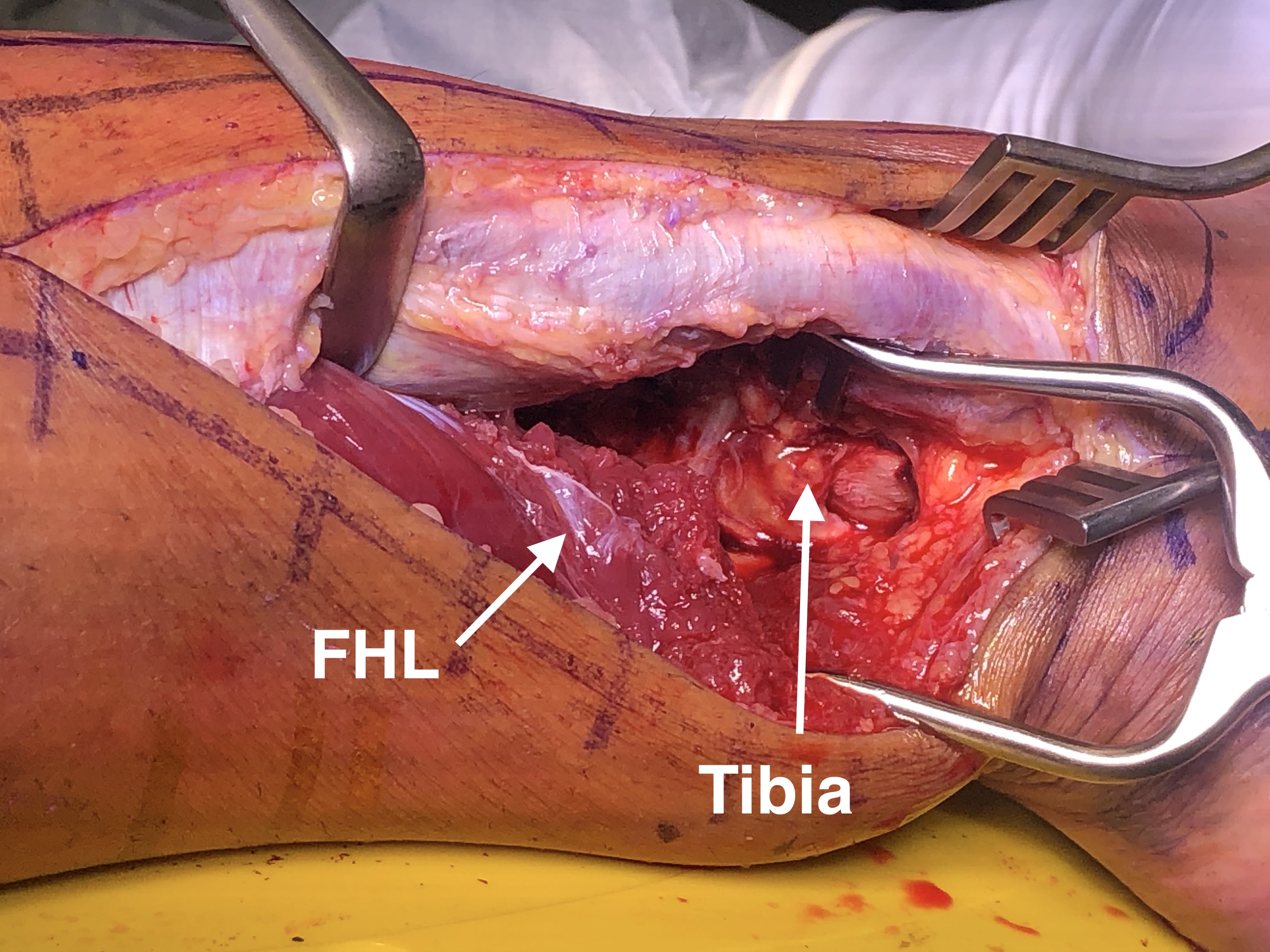
Posterolateral approach
AO Surgery Reference posterolateral approach
Vumedi posterolateral approach video
Incision between tendoachilles and fibular
- divide investing fascia
- protect sural nerve / reflect posterior
Posterior tibia
- reflect peroneal tendons anterior
- divide fascia over FHL - reflect medial
- peroneal artery is proximal on interosseous membrane deep to peroneals
Fibular
- reflect peroneals posteriorly


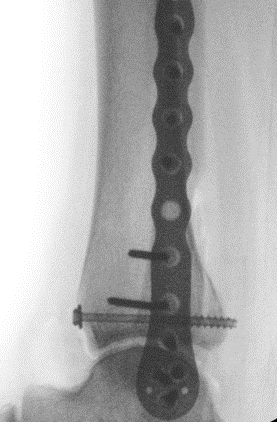
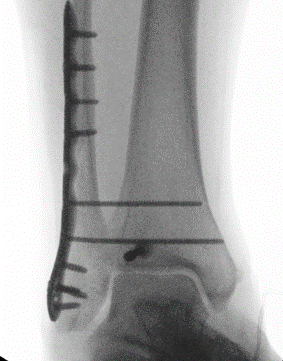
Fixation
Buttress plate
PA screws


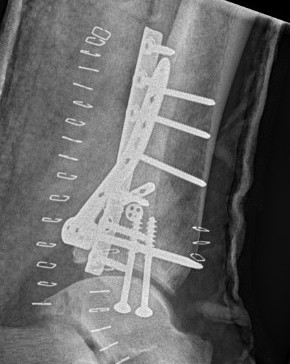
Posterolateral buttress plate


PA screws
Posteromedial approach
Indication
- posteromedial fragment

Technique
AO Surgery Reference posteromedial approach ankle
Vumedi video posteromedial approach ankle
Patient prone / supine with leg eternally rotated
Incision
- between achilles and posteromedial tibia
- divide fascia
Intervals
1. Interval between tibialis posterior and EDC
2. Interval between FDC and FHL (protect NV bundle between)



