Anatomy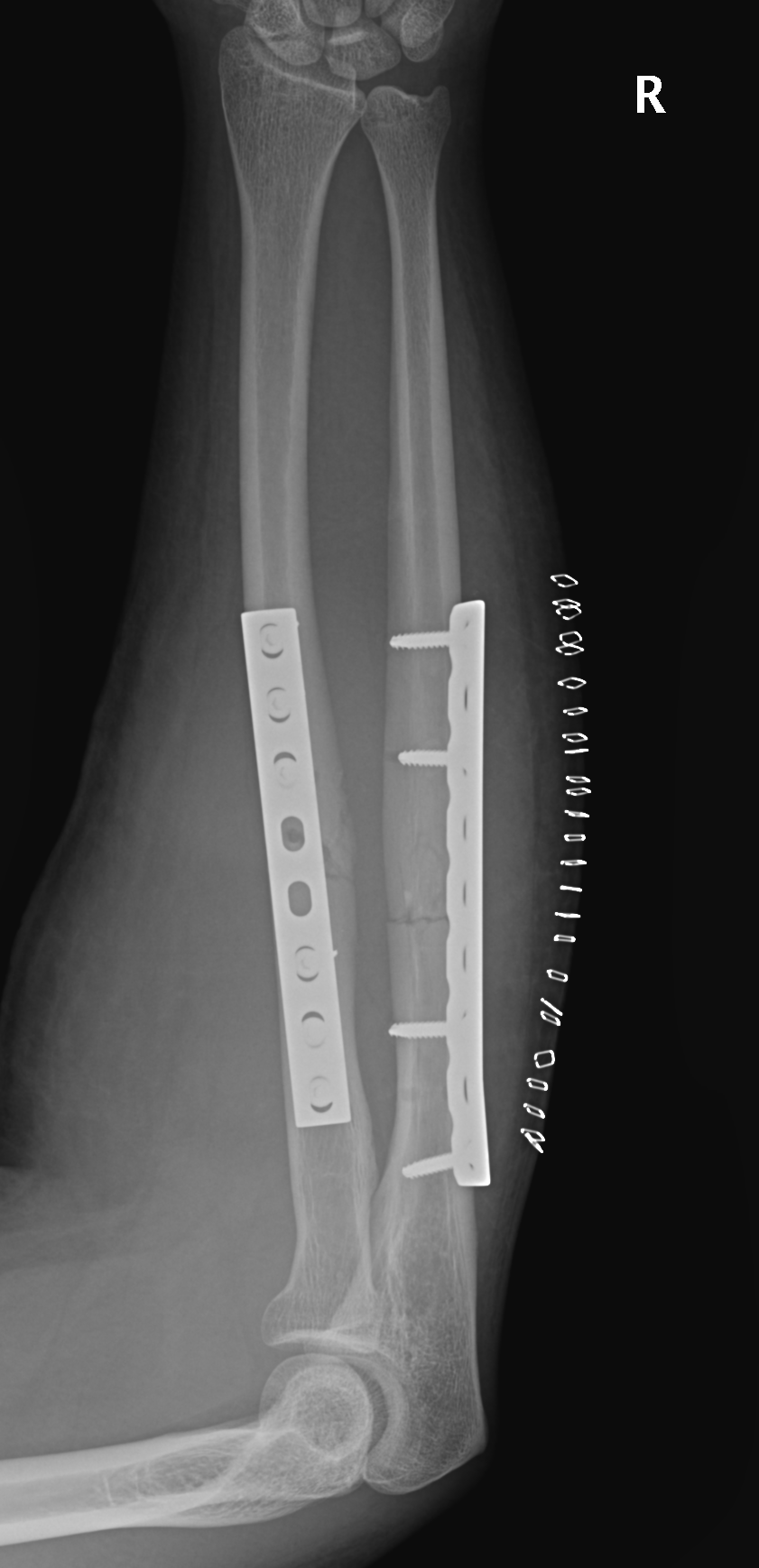
Radial bow radius
- important for rotation
Interosseous membrane
- Z pattern
- proximal radius to distal ulna
Mechanism
Direct blow
- ulna / night stick

Indirect
Monteggia
- Proximal 1/3 ulna fracture with radial head dislocation

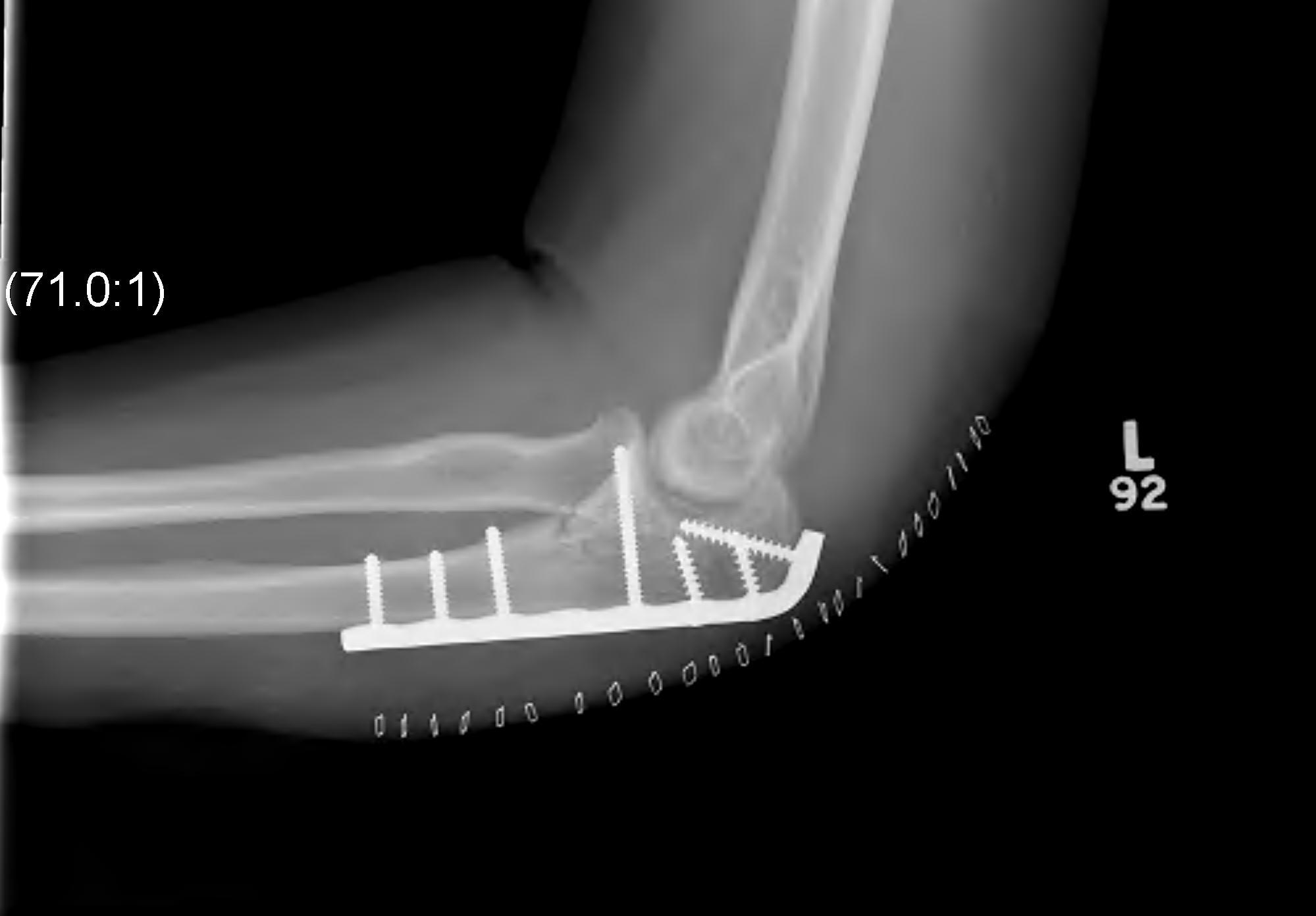
Monteggia Variant
- proximal 1/3 ulna fracture with radial head / neck fracture
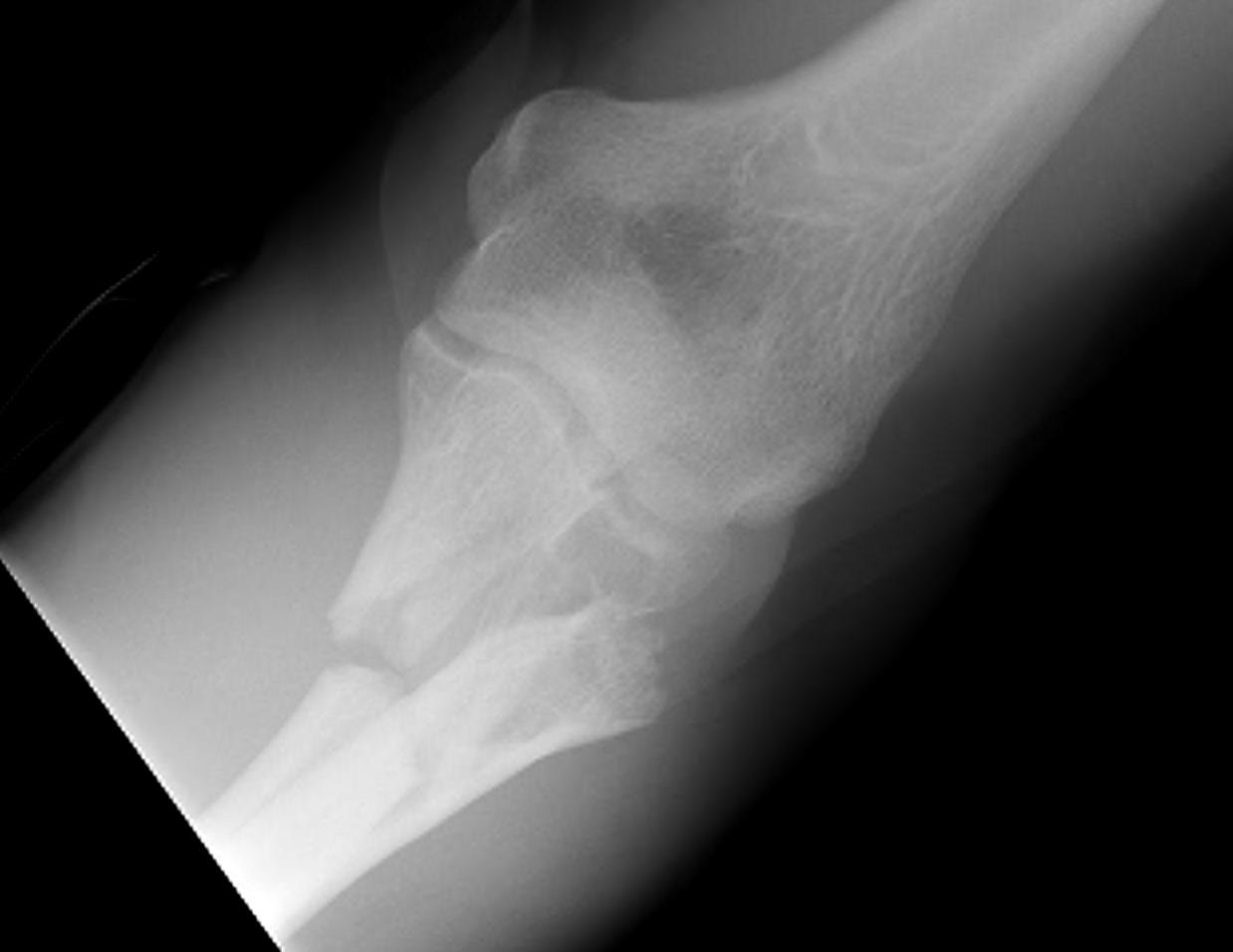

Galleazzi
- distal 1/3 radial fracture with DRUJ disruption




Both bone foream fractures


Associated Injuries
Ulna can be compound
Compartment Syndrome
X-ray
Joint above and below
Elbow
- always assess radial capitellar line on two views
DRUJ disruption
- widened space between R & U
- radial shortening > 5 mm
- ulna styloid fracture
Classification
Isolated single bone
Both bone
Fracture of one bone with ligament rupture
- Galleazzi, Monteggia
Fractures of bone bones with ligament rupture
Non operative Management
Indications
Ulna
- < 10o angulation

Radius
- completely undisplaced
- maintenance radial bow
Operative Management
Options
Intramedullary fixation
- children (good remodelling potential)
- prophylaxis to prevent pathological fracture

External Fixation
- severe injury / compound
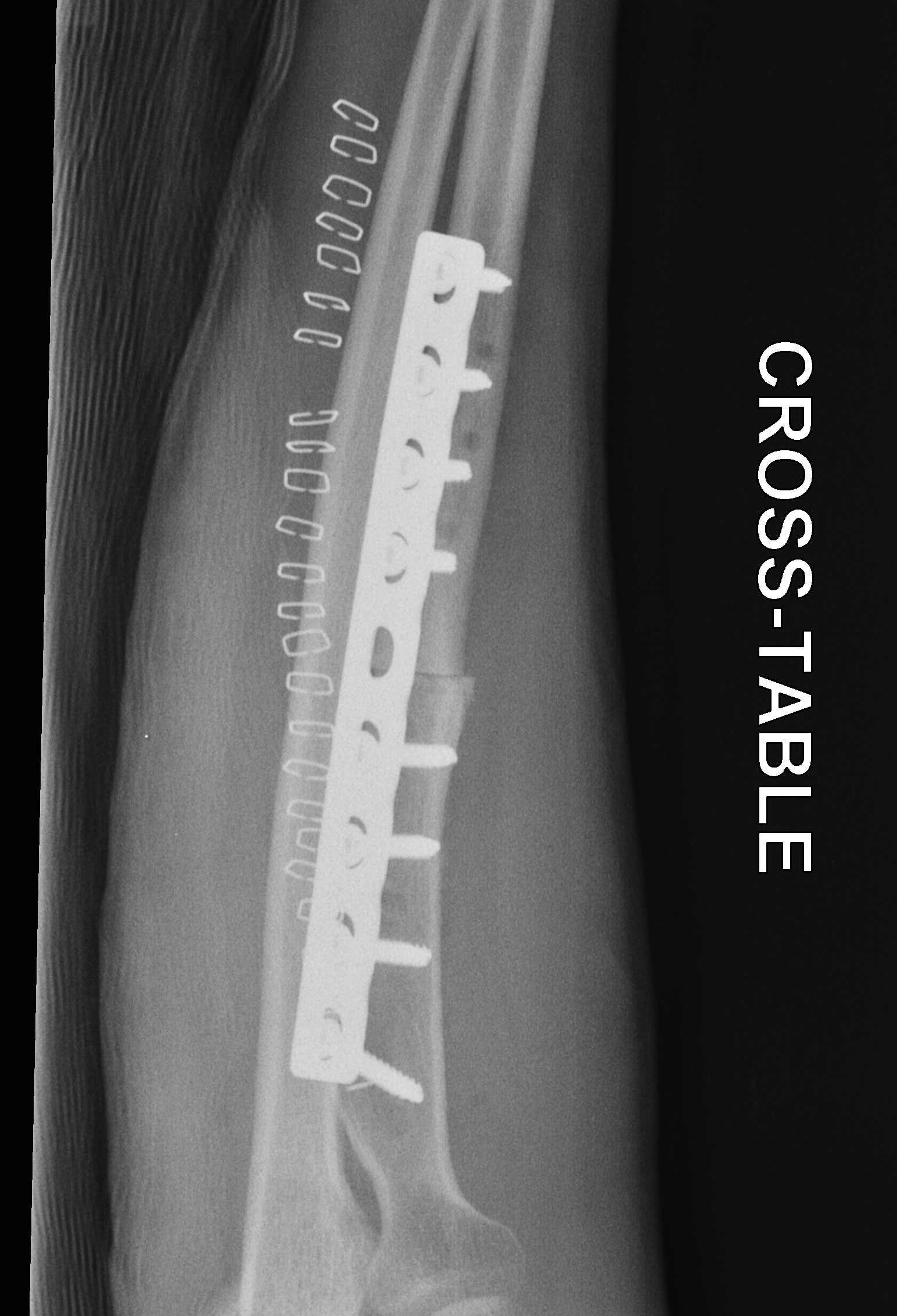
Plate fixation
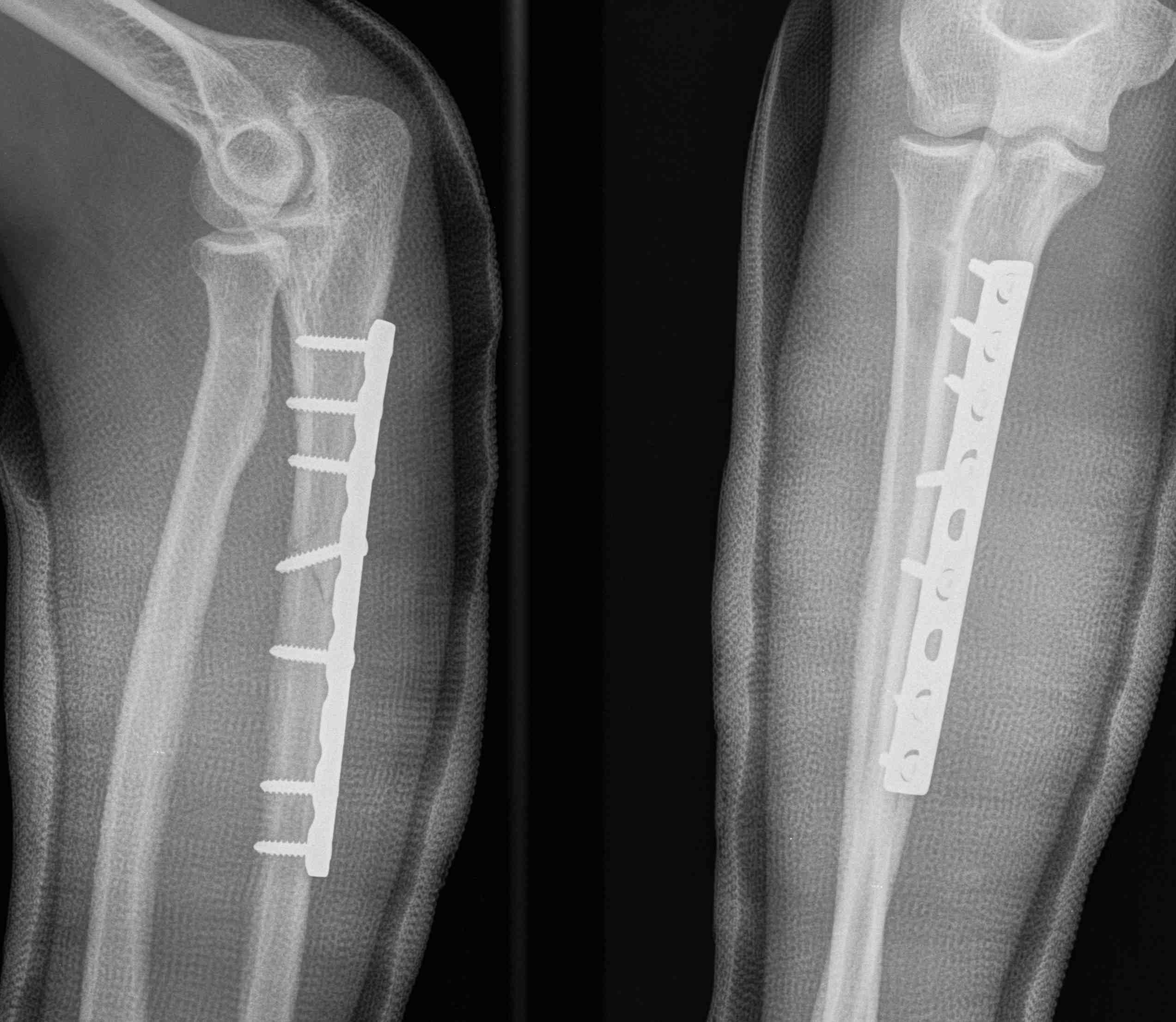
Goals
Anatomical reduction with absolute stability
- length
- rotation
- radial bow (need to bend plate for long fractures)
Approach


Ulna
- approach between ECU / FCU
Radius
Distal
- between FCR and radial artery
Proximally
- between BR and pronator teres
- supinate forearm
- elevate supinator from ulna to radial
Galleazzi
Incident DRUJ instability
- up to 50% if fracture radius < 7.5 cm to distal articular surface
- < 5% if > 7.5 cm


Plate distal radius
- assess DRUJ stability
- if stable, early ROM
- unstable, splint in supination
- if still unstable, ensure that radius is anatomical
- may have to repair TFCC / ORIF ulnar styloid
- if still unstable, may rarely have to K wire ulna to radius


Yohe et al Hand 2017
- irreducible dorsal dislocations usually due to extensor tendonds, or fracture fragments
- no soft tissue block to volar dislocations
Tsismenakis et al Injury 2017
- 7/66 (11%) incidence of DRUJ instability after fixation
- 4/7 had ulnar styloid fracture
- may need ORIF ulnar styloid / fixation of TFCC to obtain stability
- can pin DRUJ proximal to fossa
Complications
Nonunion
- 2%
- exclude infection




Malunion
Problem
- > 10o angulation leads to loss of ROM
Management
- osteotomy



Infection
Management
Initial
- excise non union
- debridement
- ABx cement spacer + external fixator
- eliminate infection
Obtain union
- BG and plate
Compartment syndrome
- don't close fascia
- good haemostasis
Synostosis
Risk factors
- fractures at same level / Monteggia
- proximal fractures
- open fractures
- head injuries
- bone grafting
- ORIF through single incision
- delayed surgery > 2 weeks
Management
Excision
- usually posterior approach
- elevate ECU from ulna
- exposes synostosis and radius
- application of bone wax to bone after debridement
- +/- irradiation / indomethacin especially in head injured patients
- worst results with proximal synostosis
